PARIS -- Clinical advances in MRI-guided percutaneous diagnosis and emerging treatment options for prostate tumors were discussed in depth during a special session at the French national radiology congress, JFR 2022.
"In the prostate, everything starts with PSA [prostate-specific antigen] determination in men at high risk of developing the disease -- men beyond 50, or 45 with a family history, and men of African descent," said Dr. Roberto Luigi Cazzato from Strasbourg, France, as he reviewed the current European recommendations.
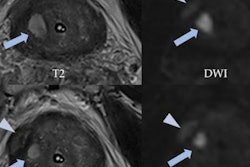
If PSA is altered, transrectal ultrasound examination will be performed, and if necessary, so will a diagnostic MR scan. "Based on all three, we'll decide whether or not to carry out biopsy, either under MR or US-MRI fusion guidance," he told JFR delegates on 7 October.
The biopsy must map the entire gland to identify the cancerous area. "With an MR-guided biopsy, everything is mapped and it's very practical," said Cazzato, who presented a recent comparative study.
"If we compare MR guidance with the more traditional technique of image fusion between US and MRI, the overall detection of cancers is equivalent," he explained. "However, the detection rate of cancers that are significant and need active management is much better with MRI guidance. We're able to better detect patients who will need surgical therapy or radiotherapy."
MR-guided biopsies remain expensive and are not widely available, but there are clear benefits in the long run. "Today prostate cancers that need active surveillance are treated by surgery or radiotherapy, and we know these come with problems, such as functional impotence and incontinence," he said.
Radiologists will be able to develop focal treatments if they can map prostate cancers properly. "We know that these treatments have the capacity to significantly reduce nerve mobility compared to whole-gland treatment, prostatectomy, or whole-gland radiotherapy," Cazzato said. "More focal treatments can be proposed without negatively impacting survival or local cancer control rates and we can treat only the significant lesions, not the whole prostate."
For the moment, MRI is very cumbersome; the final goal would be to automate these biopsies to be able to plan them ahead, according to Prof. Afshin Gangi, chairman of radiology and nuclear medicine at the University Hospital of Strasbourg and immediate past president of the Cardiovascular and Interventional Radiological Society of Europe (CIRSE).
"We need to robotize these biopsies that are done once the perineum is placed correctly and the prostate is isolated," he said at the same JFR session. "This is where we will go faster."
Transurethral ablation
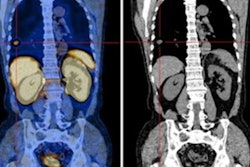
In general, there are too many treatments and too many choices in prostate cancer today, but one particularly promising transurethral ablation technique, called TULSA-PRO, involves using focused ultrasound, Gangi pointed out.
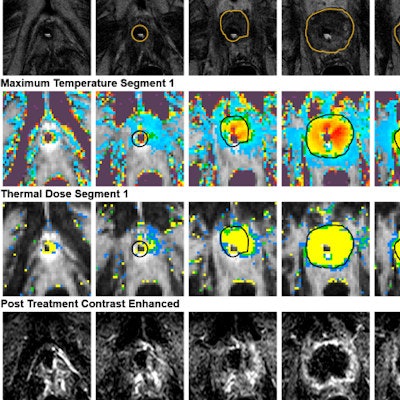
 The aim of the MRI-guided transurethral ultrasound therapy system treatment report (TULSA-Pro) is to ablate the prostate tissue of patients with localized, organ-confined cancer. Figure courtesy of Prof. Afshin Gangi.
The aim of the MRI-guided transurethral ultrasound therapy system treatment report (TULSA-Pro) is to ablate the prostate tissue of patients with localized, organ-confined cancer. Figure courtesy of Prof. Afshin Gangi.
"Urologists are very interested and looking at it very closely. As radiologists, we should also be interested, especially since it's possible to carry out the procedure during diagnostic MRI, so there's no need for sterility, etc.," he said.
TULSA, or transurethral ultrasound ablation, uses heat to target and destroy cancerous prostate tissue. It combines real-time MRI with robotically-driven directional thermal ultrasound and closed-loop temperature feedback control software, delivering transurethral prostate tissue ablation of whole-gland or partial prostate tissue, he explained.
"What I like about this technique is that the source is the center of the prostate," Gangi said. "TULSA works with ten sources of emitters, or torch lighters that rotate robotically throughout the prostate. It's a flame that shoots from the base to the periphery."
Contraindications include a prostate larger than 5 or 6 cm in diameter, as the shot is limited to 3 cm, and calcification of the gland. Another consideration is that the patient must be sedated to remain completely still.
TULSA is done in collaboration with urologists and under MRI guidance, thus providing excellent tissue contrast. Carrying out the procedure ties up a scanning room for two or three hours, but this may change soon as low-field scanners become increasingly available in clinical practice, according to Gangi.
"If we manage to make these scanners compatible with thermometry, we could use techniques such as TULSA much more often," he noted.
Technically, it is necessary to place the 10 emitters and decide where to start, either left or right. Radiologists can do that easily as they control thermometry. The probe is placed in the urethra; once the bypass is done, energy can be delivered automatically. The patient can be discharged on the next day, Gangi added.
The temperature must reach 55° C on the edges of the prostate for the procedure to be efficient. To increase the size of the ablation, a boost mode is available to increase the temperature from 57° to 65° C, but it should be used cautiously to avoid too high a temperature inside the prostate, Gangi recommended.
"I like the boost, but we must use it sparingly," he concluded.