Dynamic contrast enhancement (DCE) can help identify clinically significant cancers in prostate multiparametric MRI at 1.5 tesla, but the effect is smaller at 3 tesla and there is a higher risk of overdiagnosis due to detection of additional low-risk cancers, German researchers have reported.
"Contrast-enhanced sequences seem more important at 1.5 [tesla], and DCE may not always be necessary at 3 [tesla], especially in cases of expert reading and technically advanced diffusion-weighted sequences," radiologist Dr. Farid Ziayee and colleagues at the University of Dusseldorf noted in an article posted by the European Journal of Radiology on 13 September.
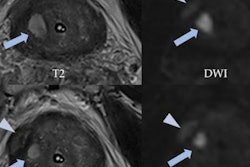
DCE may contribute to diagnostic certainty by validating the suspicious nature of a lesion seen on T2-weighted MRI and diffusion-weighted imaging (DWI), from which less experienced readers may benefit, they explained. In a previous study, the same group showed lesions that were upgraded from PI-RADS category 3 to 4 due to suspicious DCE findings, using a 3-tesla scanner, contained a substantial amount of clinically significant prostate cancers.
"PI-RADS 3 lesions are not primarily biopsied but receive follow-up [multiparametric MRI] instead so that histologic prostate cancer detection may be delayed if lesions are wrongly categorized PI-RADS 3," the authors wrote. "High sensitivity comes with the risk of over-diagnosing low-risk prostate cancer, which is to be avoided."
The impact of the magnetic field strength on the diagnostic performance of DCE in prostate cancer detection has not been fully investigated. Higher field strengths allow better image quality and may also enable a higher accuracy, especially for DWI, so DCE may be more important on 1.5-tesla than on 3-tesla scanners to compensate for the shortcomings of lower image quality in the other sequences, they pointed out.
Study details
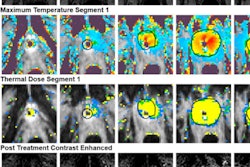
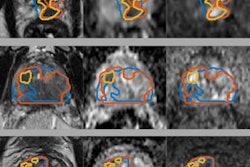
The aim of the study was to compare the amount of prostate cancer-positive lesions upgraded to PI-RADS 4 based on positive DCE findings on 1.5- and 3-tesla MRI.
In the two-center study conducted between January 2017 and March 2019, all consecutive patients classified as PI-RADS 4 in multiparametric MRI with 100 verified prostate cancers in subsequent MRI and ultrasound-guided fusion biopsy were included for 1.5- and 3-tesla MRI. Prostate cancer detection in index lesions upgraded to PI-RADS 4 based on positive DCE findings was compared between 1.5- and 3-tesla MRI.
A total of 293 patients within PI-RADS category 4 comprising 152 (mean age, 66 ± 8; median prostate specific antigen [PSA], 6.4 ng/ml; 116 peripheral zone index lesions) in the 1.5-tesla group and 141 (mean age, 65 ± 8; median PSA, 7.2ng/ml; 100 peripheral zone index lesions) in the 3-tesla group were included in the study.
The overall amount of prostate cancer (66% vs. 71%; p = 0.346) and portion of upgraded index lesions (28% vs. 21%; p = 0.126) did not differ significantly. At 1.5 tesla, prostate cancer detection was higher in upgraded peripheral lesions compared with 3 tesla (33% vs. 19%; p = 0.048).
The amount of upgraded peripheral lesions with International Society of Urological Pathology (ISUP) grade group 2-5 prostate cancer was significantly higher at 1.5 tesla versus 3 tesla (32% vs. 9%; p = 0.007). Around 33% (11/33; 1.5 tesla) and 32% (10/31; 3 tesla) of the upgraded lesions were ISUP grade group 1 prostate cancer.
The table below shows the numbers of biopsies needed to confirm one prostate cancer in upgraded lesions, subdivided into different ISUP grade groups at 1.5 tesla and 3 tesla.
| Number of biopsies needed to detect 1 prostate cancer in cases upgraded due to DCE MRI findings to PI-RADS category 4 at 1.5 tesla and 3 tesla MRI, subdivided into ISUP grade groups. | |||
| 1.5T | 3T | ||
| Targeted biopsy | Any prostate cancer | 1.5 | 2 |
| + Systematic biopsy | ISUP grade group 2-5 | 2.5 | 7 |
| ISUP grade group 3-5 | 6 | 15 | |
Given that each patient receives systematic and targeted biopsy and that more prostate cancer cases are present in the group of upgraded PI-RADS 4 patients at 1.5 tesla, the number needed to biopsy to detect one prostate cancer was lower for every subgroup in the 1.5-tesla group with a maximal difference in the subgroup of ISUP 3 to 5 verified prostate cancers (6 for 1.5 tesla vs.15 for 3 tesla), the authors wrote.
"At 1.5 [tesla], the radiologist may need to rely on the less susceptible DCE more often than at 3 [tesla], where diffusion restriction can be perceived more easily," they noted. "Without contrast medium, there would have been a significant amount of clinically significant prostate cancer that would have been classified as PI-RADS 3 at 1.5 [tesla] and where biopsy may have been postponed or waived depending on the respective in-house standard."
Some positive PI-RADS 4 lesions that did not need an upgrade based on DCE at 3 tesla may not have been that obvious at 1.5 tesla and may have needed an upgrade via DCE. This may explain the larger amount of clinically significant cancers in upgraded lesions at 1.5 tesla.
The amount of low-grade cancer in upgraded lesions did not differ markedly between the two field strengths.
"The reason for this may be the fact that low-grade prostate cancers tend to exhibit rather discrete imaging changes and higher grade cancers tend to exhibit strong signal changes in multiparametric MRI. Hence, low-grade tumors may be harder to detect at 1.5 [tesla] and at 3 [tesla] compared to high-grade prostate cancers and may require DCE at both magnetic field strengths," they concluded.