Radiomics features extracted from multiparametric MRI exams can help predict whether prostate cancer will metastasize, according to research presented at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting in London, U.K.
The findings illuminate how prostate cancer circulating tumor cells negatively affect patient outcomes, presenter Mohammad Alhusseini, PhD, of the University of Miami Miller School of Medicine in Florida noted.
"Circulating tumor cells are cancer cells detectable in the peripheral blood released by the tumor," he said. "[They] constitute seeds for subsequent growth of additional tumor metastases, triggering a mechanism that is responsible for many cancer-related deaths."
The ISMRM is holding this week's meeting in conjunction with the European Society for Magnetic Resonance in Medicine and Biology and the International Society for MR Radiographers and Technologists.
An indicator of prostate cancer risk
The number of circulating tumor cells (CTCs) is an indicator of metastatic risk in prostate cancer and is a meaningful biomarker, the team explained.
"Quantitative multiparametric MRI features in prostate cancer are associated with tumor aggressiveness," Alhusseini said.
The investigators explored any links between radiomic features from multiparametric MRI of the prostate and circulating tumor cell counts in 73 prostate cancer patients. They developed and trained a neural network algorithm to predict circulating tumor cell counts (with a threshold of five or more CTCs indicating risk of metastatic disease). The team conducted 100 training and testing runs of five-fold cross-validation, measuring results using the area under the receiver operating curve (AUC).
The team used the following radiomics features to train the algorithm:
- "T-onset" -- time of onset of the contrast wash-in
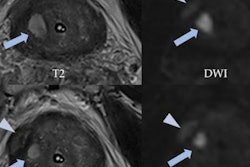
- T2 intensity, 50%
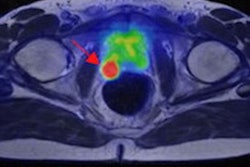
- Higher tumor volume, measured by a tool the group developed for the algorithm called the Habitat Risk Score 6 (HRS6), which is based on a one to 10 scale ("Volumes with HRS6 are concordant with tumor volumes from radical prostatectomy samples," the authors wrote in their abstract.)
- Apparent diffusion coefficient (ADC) intensity skewness
- ADC contrast mean
- ADC contrast kurtosis
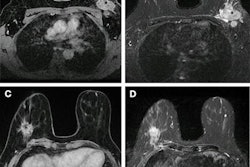
- B-value intensity
Alhusseini's group collected blood from study participants enrolled in two trials: one an "active surveillance" trial and another a randomized radiotherapy trial that investigated the effects of an MRI-guided prostate radiotherapy treatment. Patients underwent multiparametric MRI (including axial T2-weighted MRI, diffusion-weighted imaging [DWI] and dynamic contrast-enhanced [DCE]-MRI exams) and MRI-ultrasound fusion biopsy. The amount of circulating tumor cells was assessed from the blood draws.
In the active surveillance trial arm, the mean circulating tumor count per 7.5 mL of blood was 19. In the radiotherapy trial arm, the median circulating tumor count in 7.5 mL of blood was 74.
Using the seven features, the team found an average AUC of 0.769 for a connection with higher CTC counts and adverse effects; of the seven, HRS6, lower T2 intensity measurements, and time of onset were the top three, with an AUC of 0.834.
"To the best of our knowledge, this is the first study to model CTC counts with in vivo multiparametric MRI radiomics," the group concluded. "Magnetic resonance imaging radiomics features are promising markers of prostate cancer metastatic risk."