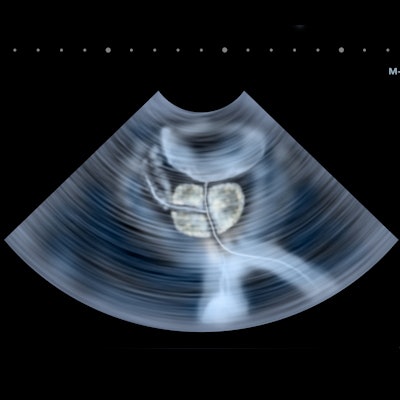
A nomogram prediction model that uses contrast-enhanced ultrasound (CEUS) can help predict prostate cancer risk in men, a Chinese study published on 25 July in the British Journal of Radiology found.
Researchers led by Dr. Yunyun Liu from Tongji University developed the model, which also uses age and the Prostate Image and Reporting Data System (PI-RADS). The model showed a higher area under the curve (AUC) than control models.
"This study showed that PI-RADS v2.1 and CEUS were significant predictors of prostate cancer and clinically significant prostate cancer in patients with 'gray zone' prostate-specific antigen levels," Liu et al wrote.
Prostate-specific antigens are one of the most important biomarkers of prostate cancer, with biopsy being the gold standard for confirming prostate cancer diagnosis. However, there is a persistent concern about patients undergoing an unnecessary biopsy, especially in men with "gray zone" antigen levels (4-10 ng/mL).
While multiparametric MRI has been proposed to help manage prostate cancer, the researchers noted issues with accessing this technology. This includes the lack of qualified MRI scanners and sufficiently experienced radiologists.
CEUS has also demonstrated high sensitivity and specificity in previous research but is currently not recommended for use in combination with MRI. The study authors wrote that this is partly due to weaknesses in intraobserver and device-dependent interobserver reliability.
Liu and colleagues wanted to test the waters by creating a prediction model based on PI-RADS version 2.1 (PI-RADS v2.1) and CEUS for predicting both clinically significant and insignificant prostate cancer in men. The model is represented by a nomogram, a diagram representing relations between variables. The end goal was to avoid unnecessary biopsy for men whose prostate-specific antigen levels were in the gray zone.
The authors tested the model on 490 men who underwent prostate biopsy for prostate-specific antigen levels from 4-10 ng mL−1. The patients were randomly divided into a pilot cohort (70%) and a validation cohort (30%).
The team found that age, PI-RADS score, and CEUS findings were independently tied to prostate cancer and clinically significant prostate cancer. This meant the nomogram could better discriminate between the two.
| Performance in AUC of nomogram using CEUS to identify prostate cancer | |
| Type of cancer | AUC |
| Prostate cancer (pilot cohort) | 0.843 |
| Clinically significant prostate cancer (pilot cohort) | 0.876 |
| Prostate cancer (validation cohort) | 0.818 |
| Clinically significant prostate cancer (validation cohort) | 0.857 |
The researchers also found that the nomogram's diagnostic performance was comparable to a second model they explored that included all available parameters (p > 0.05). The nomogram also showed "meaningful" reduction in unnecessary biopsy rate, from 74.8% to 21.1% in prostate cancer, and from 83.7% to 5.4% in clinically significant prostate cancer.
While the team called for validation studies with larger cohorts, they also wrote that using CEUS in their model can lead to "meaningful reduction" in the number of unnecessary biopsies.