
Ultrasound is providing useful clinical information about the impact of COVID-19 infection on the thyroid, and it shows that the disease can cause atypical thyroid inflammation, Italian researchers have reported.
Thyroiditis during moderate-to-severe COVID-19 is painless, which is different from classic viral subacute thyroiditis, Dr. Ilaria Muller, PhD, lecturer in endocrinology at the department of clinical sciences and community health at the University of Milan, told AuntMinnieEurope.com ahead of her presentation on the topic at ENDO 21, the Endocrine Society's annual meeting, which was held virtually between 20 and 23 March.
Therefore, in their paper posted online on 30 July 2020 by Lancet Diabetes Endocrinology ("SARS-CoV-2-related atypical thyroiditis"), the group referred to this thyroiditis as atypical, she added.
Usually classic subacute thyroiditis affects women, while COVID-19 disease, and consequently such atypical thyroiditis, predominantly affects men, according to Muller. Although other viral infections such as mumps, influenza, adenovirus, and coxsackievirus can cause subacute thyroiditis, they are not routinely tested for, and ultrasound of thyroiditis caused by a viral infection often shows up as "massive hyperechoic areas, and sometimes they migrate, so they can change from one position to another."
Classic subacute thyroiditis has also been described after SARS-CoV-2 infection of mild entity, and it is associated with typical neck pain and is more frequent in women, Muller noted.
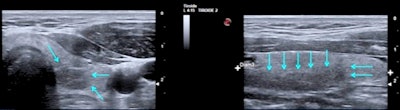 A 46-year-old man two to three months after COVID-19 infection. Thyroid ultrasound scan in transverse (left) and longitudinal (right) planes shows presence of focal hypoechoic area (arrows) suggestive of thyroiditis in left thyroid lobe, inferior and posterior position. All figures courtesy of Dr. Ilaria Muller, PhD, presented at ENDO 2021.
A 46-year-old man two to three months after COVID-19 infection. Thyroid ultrasound scan in transverse (left) and longitudinal (right) planes shows presence of focal hypoechoic area (arrows) suggestive of thyroiditis in left thyroid lobe, inferior and posterior position. All figures courtesy of Dr. Ilaria Muller, PhD, presented at ENDO 2021."When you perform the first ultrasound in sub-acute thyroiditis, you've got the big hyperechoic areas, then you usually start steroid treatment and despite the neck pain disappearing, when you repeat the ultrasound after one month, two months, the areas are still there and they take months to disappear," She said.
Bearing in mind such behavior of classic subacute thyroiditis, she said she did not find it surprising that hypoechoic areas of atypical thyroiditis related to COVID-19 also persisted after two to three months. Furthermore, the whole thyroid gland was a little more dishomogeneous and showed a diffusely hypoechoic pattern compared to a normal thyroid, although she said it was quite difficult to standardize in the ultrasound machine settings.
Latest findings in Milan
In spring 2020, 15% of the COVID-19 patients hospitalized in acute medicine units at Milan's Fondazione IRCCS Ca' Granda Policlinico Hospital in Italy had thyroid hormone alterations due to multifactorial causes, including thyroid inflammation, Muller told ENDO 21 registrants. In comparison, only 1% of hospitalized patients during the same period in 2019 prior to the pandemic had thyroid hormone alterations.
During the first wave of the pandemic, baseline investigations of patients on admission to hospital were conducted. They showed that many of the seriously affected patients who required a high level of subintensive care had a low or suppressed level of serum thyroid-stimulating hormone, possibly as a consequence of atypical subacute thyroiditis induced by SARS-CoV-2, Muller noted.
 Thyroid ultrasound scan (longitudinal plane) of a 73-year-old man with COVID-19. Left: three months after infection. Presence of a focal hypoechoic area (arrows) suggestive of thyroiditis in his right thyroid lobe, inferior and posterior position. Right: six months postinfection, the hypoechoic area is still there, but much reduced in size.
Thyroid ultrasound scan (longitudinal plane) of a 73-year-old man with COVID-19. Left: three months after infection. Presence of a focal hypoechoic area (arrows) suggestive of thyroiditis in his right thyroid lobe, inferior and posterior position. Right: six months postinfection, the hypoechoic area is still there, but much reduced in size.Muller and colleagues started a surveillance program to monitor the thyroid function of patients every three months after being hospitalized for moderate to severe COVID-19 disease. The patients undergo routine blood and ultrasound testing using a MyLab 25Gold ultrasound scanner from Esaote to monitor their thyroid function and signs of inflammation.
A total of 53 patients (60% men, mean age 61 ± 10 years) have so far completed the evaluation at three months. All of them had normalized thyroid function, but the team found the thyroiditis in people with moderate to severe COVID-19 disease differs from typical thyroiditis in several ways. These include the absence of neck pain, the presence of mild thyroid dysfunction, higher frequency among men, and the association with severe COVID-19 disease.
One-third of the study participants still had signs of thyroid inflammation after three months, even though their thyroid function had normalized. The study is following patients to determine whether this inflammation will trigger permanent thyroid dysfunction or autoimmunity.
Muller explained that while she expected to see a frequent occurrence of hypothyroidism, following classic subacute thyroiditis, she said that the degree of thyrotoxicosis observed during COVID-19 has undoubtedly been milder than that occurring during classic viral thyroiditis.
"Based on that, you would not expect such significant persistent thyroid damage, so it has not been surprising that we didn't see that after three months," she said. "However, we know that hypothyroidism can occur in the mid to long term, so this is why we are continuing to study these patients.
"Also, antibodies to the thyroid gland might become positive, because any kind of damage to the thyroid can trigger autoimmunity. So we might see a rise of these antibodies later on and trigger autoimmunity."
Because the study started predominantly during the first wave of the pandemic, there were stringent restrictions to prevent the disease from spreading. Therefore, before being able to recall patients for ultrasound, the group needed to wait two to three months from the baseline thyroid function assessment when COVID-19 was diagnosed. Scans were performed two to three months from the onset of disease, and the team had to wait for patients to be discharged and to have a negative COVID-19 swab.
Endocrinologists and ultrasound
Muller also described the use of ultrasound by specialty in different regions of Europe. She said many Italian endocrinologists perform thyroid ultrasound, so in this study, only endocrinologists carried out the ultrasound scans. No radiologists were involved.
Having worked in the Thyroid Research Group at the Division of Infection & Immunity, Cardiff University, U.K., for six years, she said she was initially surprised that radiologists and not endocrinologists performed thyroid ultrasound. In Italy, endocrinologists are trained to perform thyroid ultrasound, which is a routine part of patient investigation.
Overall, the researchers suggest routine assessment of thyroid function in patients with COVID-19 requiring high-intensity care because often they present with thyrotoxicosis due to a form of subacute thyroiditis related to SARS-CoV-2. Further studies are needed to confirm, or counter, these results, and the researchers think thyroid cytology or histology and longitudinal studies of thyroid (dys)function in these patients would be useful.



















