Automated assessment of ground-glass opacities on lung CT exams in patients with suspected COVID-19 patients correlates well with clinical outcomes and shows potential as an objective biomarker for evaluating the severity of lung injury, according to research published online on 13 November in Anaesthesia Critical Care & Pain Medicine.
In a retrospective study, a team of researchers from Strasbourg University Hospital in France led by Dr. Eric Noll found that their automated approach for measuring the volume of ground-glass opacities yielded similar results to semiautomated segmentation and was much faster. What's more, it also correlated well with clinical outcomes for patients over the seven days following their CT exams.
"This automated quantitative analysis could be widely implemented, could be used clinically to aid with diagnosis, and can be used in clinical research as an objective and quantitative measure of severity of lung injury for eligibility assessment, primary or secondary endpoints, or as a potential confounder of disease severity," the authors wrote.
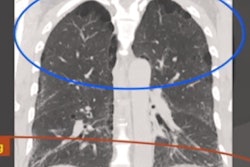
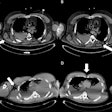
As ground-glass opacities are an important radiological feature of SARS-CoV-2 infections, the researchers sought to assess the feasibility of an automated and quantitative measure of ground-glass opacities on lung CT images that could serve as an objective measure of lung injury severity for both clinical and research use in COVID-19 patients.
"We hypothesized that automated quantification of ground-glass opacity is feasible and that more lesions are associated with worse clinical outcome," they wrote.
The researchers gathered CT images, demographic data, and respiratory treatment information in a study involving 38 patients with COVID-19. Of the 38 patients, 17 were admitted to the intensive care unit (ICU) and 21 were non-ICU patients.
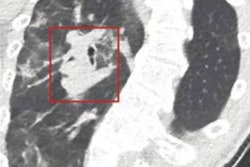
Next, Noll and colleagues measured the volume of abnormal lung parenchyma both with conventional semiautomatic segmentation software and with a novel automated algorithm based on voxel x-ray attenuation. An expert senior clinical radiologist validated the anatomical results of the lung parenchyma segmentations in all cases.
Using clinical data abstracted from the electronic medical record for each patient, the authors assessed the disease maximal severity based on a seven-category ordinal scale during the seven days after the CT exam. They then compared these findings with the automated and semiautomated segmentation results.
The team found that the volume of restricted normally aerated lung volumes was significantly lower in the ICU patients compared with the non-ICU patients, for both the semiautomated (p = 0.048) and automated measurements (p = 0.045). The intraclass correlation coefficient between both methods was 0.99 for ground-glass opacities and restricted normally aerated lung. However, the automated measurements took only 15 minutes to calculate, compared with 93 minutes for the semiautomated approach.
Importantly, the researchers found that the association between the automated measured lung volume and the maximal clinical severity score was statistically significant for the restricted normally aerated (p = 0.0097, effect size = -385 mL) volumes, as well as for the ratio of ground-glass opacities/restricted normally aerated volumes (p = 0.027, effect size = 3.3).
"This radioclinical assessment for impaired lung volume measurement is a promising concept for various medical fields including infectious diseases, perioperative medicine, and critical care," they wrote.
As the study involved a small number of patients, these preliminary findings will need to be confirmed in a larger sample size, the authors noted.