Misconceptions about COVID-19 remain widespread, leading Dutch researcher Prof. Dr. Matthijs Oudkerk, PhD, has emphasized. He calls for a change of thinking to take account of new discoveries related to the vascular aspects of the disease and for a well-informed discussion about the optimum use of CT.
"It's strange that at the moment, still there is a major opinion that [COVID-19] is just comparable with a common flu, and it is still regarded as a pulmonary infection," he said in a podcast posted by the British Institute of Radiology (BIR). "We should realize that this is a new disease, with a new syndrome, and it should be treated differently."
 Prof. Dr. Matthijs Oudkerk, PhD.
Prof. Dr. Matthijs Oudkerk, PhD.Oudkerk, professor of radiology at the University of Groningen and chief scientific officer at the Institute of Diagnostic Accuracy in Groningen, thinks the general view was -- and still is -- that COVID-19 is a primary pulmonary infection affecting the respiratory tract complicated by classic deep vein thrombosis and pulmonary embolism. However, the multidisciplinary report published in April by the National Institute for Public Health of the Netherlands postulated that the ARDS (acute respiratory distress syndrome) in COVID-19 was not simply caused by impaired ventilation but primarily by impaired pulmonary perfusion as a result of microvascular obstruction.
The document included guidance on diagnosis, prevention, and treatment of thromboembolic complications in COVID-19, as well as the angiotensin converting enzyme 2 (ACE2) theory and evidence supporting it and how this theory may change management of COVID-19 patients, he explained.
Oudkerk, founder and past president of the European Society of Cardiac Radiology, noted that COVID-19 viral infection induces a complete vascular disease syndrome that initiates a viral attack on the ACE2 receptors of the microvasculature system, resulting in two distinct processes: microvascular thrombosis and inflammation of the endothelium.
"It is important from the very beginning to start with therapy that is focusing on the development of thrombi," he said. "In the Netherlands we also treat, at the same time, the inflammatory response so we give a combination of prophylaxis and anti-inflammatory drugs."
Imaging aspects
The radiological features of the lungs at disease onset are bilateral ground-glass opacities (GGOs) and vessel enlargement in almost all cases, and these findings can be explained by the subacute flow redistribution as a result from the microvascular obstruction and pulmonary thrombosis, expressing interstitial edema and hyperemia circumventing the thrombosed, normal ventilated pulmonary lobules, according to Oudkerk. This matches with postmortem results where transudate is found as a result of the vascular obstruction and congestion and not exudate fluid as one would expect in pulmonary inflammation.
"All this evidence proves the vascular impact of COVID-19 causing an endothelial vasculitis and microvascular thrombosis at the moment it attacks the ACE2 receptor of the vessels, resulting in a process of thrombo-inflammation in the disease onset and therefore cannot be regarded as just a complication of COVID-19. Studies have shown that anticoagulants have a substantial positive impact on outcomes in COVID-19," he continued.
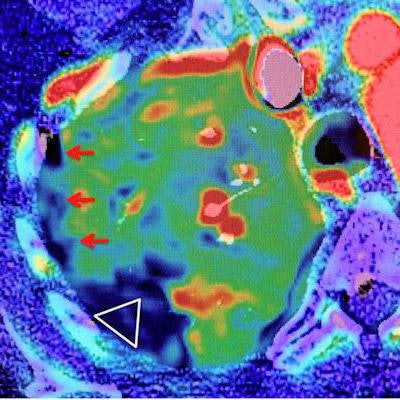
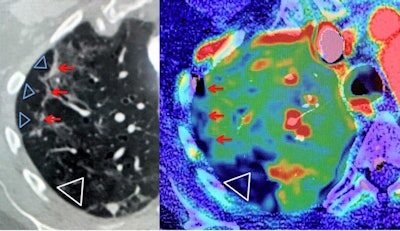 Chest CT perfusion angiography in COVID-19. A COVID-19 positive-tested 54-year-old woman presented with fever and dry cough lasting 10 days, with clinical suspicion of pulmonary embolism. Left image: Chest baseline CT of the right upper lobe with subpleural bands of organizing pneumonia (red arrows), surrounded by small ground-glass opacities (GGOs). Right image: CT perfusion angiography image shows multiple small subpleural perfusion defects (red arrows) and a larger perfusion defect dorsal in the normal ventilated right upper lobe (Δ on left image), due to microvascular obstruction (Δ on the right image). CT angiography showed no pulmonary emboli in the right pulmonary upper lobe, resulting in perfusion/ventilation mismatch. Scan parameters: conventional dynamic perfusion CT, Somatom Drive, Siemens; scan volume 8.4 cm (aorta arch -- left atrium); 1 mm recon; dual input lung perfusion 4D, Vitrea, Vital, Canon. Courtesy of BJR and department of radiology, Haaglanden Medical Centre, The Hague, the Netherlands.
Chest CT perfusion angiography in COVID-19. A COVID-19 positive-tested 54-year-old woman presented with fever and dry cough lasting 10 days, with clinical suspicion of pulmonary embolism. Left image: Chest baseline CT of the right upper lobe with subpleural bands of organizing pneumonia (red arrows), surrounded by small ground-glass opacities (GGOs). Right image: CT perfusion angiography image shows multiple small subpleural perfusion defects (red arrows) and a larger perfusion defect dorsal in the normal ventilated right upper lobe (Δ on left image), due to microvascular obstruction (Δ on the right image). CT angiography showed no pulmonary emboli in the right pulmonary upper lobe, resulting in perfusion/ventilation mismatch. Scan parameters: conventional dynamic perfusion CT, Somatom Drive, Siemens; scan volume 8.4 cm (aorta arch -- left atrium); 1 mm recon; dual input lung perfusion 4D, Vitrea, Vital, Canon. Courtesy of BJR and department of radiology, Haaglanden Medical Centre, The Hague, the Netherlands.Direct contrast CT visualization of thrombi in the postcapillary pulmonary veins remains difficult because it is beyond CT visualization thresholds with current technology.
"As a consequence, pulmonary thrombosis is at this dark side of the moon," he said. "CT perfusion angiography would be a powerful tool to demonstrate pulmonary perfusion defects, but is an advanced CT technique and still not routinely available."
Dual-energy CT reflects only the contrast-enhanced blood pool in steady state without a temporal component. Noncontrast CT can detect the very early signs of pulmonary microvascular thrombosis by the typical presentation of GGOs and vessel enlargements even before the PCR test becomes positive. In the vast majority of these patients, D-dimer levels are < 1000 ng/ml. They can be sent home safely as soon as symptoms allow. In those with plasma D-dimer > 1000 ng /ml, preventive and therapeutic anticoagulation should start immediately, and D-dimer monitoring is indicated.
"The situation is quite alarming," he said. "We think that CT should play a major role because CT can precede the diagnosis before the PCR (polymerase chain reaction) test, so the COVID-19 tests become positive. That means CT also monitors the disease development very closely. We have to develop this in such a short time."
The normal process of gathering evidence for treatments and diagnosis in medical research cannot be done in a pandemic, and that really hampers finding a standardized way for the entire world. Also important are the substantial differences between populations.
"There are different approaches in different countries -- for example, in the U.S. they think that with pneumonia, CT is not indicated, so it's very hard to do any research in the U.S. at this level with CT in the COVID-19 population," noted Oudkerk, adding that the strategy should be tailored to the specific country, the population, and the techniques available.
Patients with stable chest pain
A second BIR podcast posted on 30 October focuses on imaging patients with stable chest pain, and it features a 28-minute interview with Oudkerk and Prof. Edwin van Beek, SINAPSE chair of clinical radiology and honorary consultant radiologist at NHS Lothian Health Board, U.K.
"CT will have a dominant position in the analysis of the cardiac (system) as a whole, including valve diagnostics, including the myocardium in due time, but for very special and dedicated questions where tissue characterization is key for the diagnosis, MR will be the method to perform this part of the analysis," Oudkerk said.
Both podcasts can be downloaded free-of-charge from the BIR website. Also, Oudkerk and van Beek have guest-edited a collection of articles on the theme of imaging patients with stable chest pain.
“This special feature marks the moment of publication of the first hard evidence that non-invasive coronary CT imaging in patients with chest pain saves lives compared to current medical practice and at the same time is a lot less harmful for the patient, costs less and is more effective,” Oudkerk stated.
The collection includes articles about the potential for functional coronary and cardiac CT imaging beyond the evaluation of the coronary artery lumen, the potential role of noncardiac findings in risk stratification, and the role of machine learning to drive forward enhanced imaging data analysis.
"In addition, the role of MRI for the assessment of chest pain is of great importance, as is the role of imaging in the evaluation of heart valve disease," he pointed out. "Lastly, novel methods for the evaluation of heart viability and coronary artery disease, with a focus on developing ways to assess vulnerable plaque are coming to the fore and are reviewed."