A large study of hospitalized COVID-19 cases at three university hospitals in Dublin has found an incidence rate of over 22% of pulmonary embolism (PE) in those patients undergoing CT pulmonary angiography (CTPA). The full results are being presented at ECR 2021, which begins today.
The development of a pulmonary embolus and a raised D-dimer level were associated with an increased risk of death, and in men, a raised D-dimer level and severity of COVID-19 lung parenchymal changes were associated with an increased risk of admission to the intensive care unit (ICU), according to Dr. Roisin Heaney, specialist registrar in radiology at St. James's Hospital in Dublin, and colleagues.
"Thrombotic complications including PE, deep vein thrombosis, ischemic stroke, and myocardial infarction have become increasingly apparent and contribute to high morbidity and mortality rates," they noted in an e-poster. "The incidence of PE in patients with COVID-19 undergoing CTPA ranges from 18% to 33%. The overall prevalence in patients with COVID-19 remains unclear, with incidental PE frequently identified on postmortem examinations."
A total of 925 patients underwent CTPA for the investigation of suspected pulmonary embolus between 6 March 2020 and 22 May 2020 at three tertiary referral hospitals in Dublin: St James's Hospital, Tallaght University Hospital, and Mater Misericordiae University Hospital. The authors identified patients who were reverse transcription polymerase chain reaction (RT-PCR) positive for SARS-CoV-2 on nasopharyngeal swab. They recorded gender, age, CTPA result, D-dimer, ICU status, and deaths.
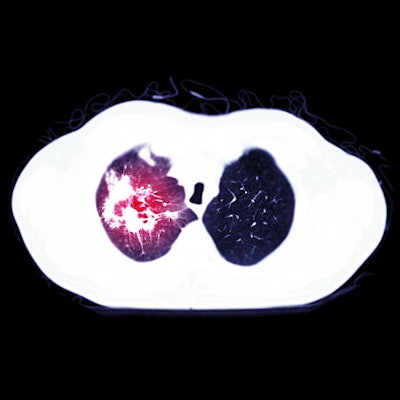
Heaney and colleagues evaluated each CTPA for the presence of an acute filling defect in the pulmonary vasculature, and the patients were divided into two groups: PE or no PE. They also assessed all CT scans for parenchymal findings consistent with COVID-19, primarily ground-glass opacities (GGOs), GGOs and septal thickening (crazy-paving appearance), and airspace consolidation.
The authors looked at the number of involved lobes and the degree of involvement of the worst affected lobe. They divided degree of involvement into five categories: none (0%), < 25%, 25%-50%, 50%-75%, and > 75% parenchymal involvement. They studied all CTs for the presence of mediastinal or hilar adenopathy, deeming adenopathy to be present if lymph nodes measuring greater than 1 cm in short axis were identified in the lung hilar or mediastinum.
Of the 925 patients, 116 were RT-PCR-positive for SARS-CoV-2. Two studies were not of diagnostic quality and were repeated, and 26 patients had a positive study for pulmonary embolus (22.4%) versus 90 patients (77.6%) who had negative studies.
| Patient demographics, D-dimer results, and outcomes | |||
| All patients | PE | No PE | |
| Age | |||
| Mean | 59.3 | 61.7 | 58.6 |
| Range | 17-99 | 26-86 | 17-99 |
| Standard deviation | 16.8 | 13.7 | 17.6 |
| Gender | |||
| Male | 71 (61.2%) | 18 (69.2%) | 53 (58.9%) |
| Female | 45 (38.8%) | 8 (30.8%) | 37 (41.1%) |
| D-dimer (ng/mL) | |||
| Mean | 3,645 | 8,169 | 2,352 |
| Range | 215-20,000 | 1,030-20,000 | 215-10,000 |
| Standard deviation | 4,549 | 6,942 | 2,391 |
| Outcomes | |||
| COVID-19 lung changes | 97 (83.6%) | 23 (88.5%) | 74 (82.2%) |
| Lymphadenopathy | 47 (40.5) | 14 (54%) | 33 (37%) |
| ICU admission | 47 (40.5%) | 11 (40.7%) | 36 (40.4%) |
| Death | 16 (13.8%) | 7 (25.9%) | 9 (10.1%) |
A total of 71 patients were men (61.2%) and 45 were women (38.8%), and there was no significant difference in gender between the PE and the no PE groups. The mean age was 59.3 (range, 17-99 years). The mean age was higher in those with a PE (61.7 years) than those without PE (58.6 years) (p = 0.28).
A D-dimer test was performed on 108 of the 116 patients (93%) within 48 hours of the CTPA. The mean D-dimer was 3,645 ng/mL, ranging from 215-20,000 ng/mL. The mean D-dimer was significantly higher in those with a positive study (8,169 ng/mL) versus the negative study group (2,352 ng/mL) (p < 0.001). All patients in the positive group had a D-dimer in excess of 1,000 ng/mL.
In total, 47 patients required admission to the ICU (40.5%) and 16 patients did not survive (13.8%). Of those with PE on CTPA, seven patients did not survive (26.9%) (p = 0.028). There was no significant difference in rates of ICU admission between the PE groups. Men were more likely to require ICU admission, accounting for 77% of patients (p = 0.005). A high D-dimer result was also associated with increased rates of ICU admission (p = 0.045) and death (p < 0.001).
Imaging findings
In the 26 patients who had a PE, the most common location of the acute PE was a segmental branch (61.5%).
A total of 97 patients (83.6%) had parenchymal changes deemed typical of COVID-19 on CT. The table below demonstrates the distribution of the lung changes by lobe and the percentage involvement of the worst affected lobe. The researchers found no significant difference in the parenchymal changes between the PE and no PE groups.
| Distribution of parenchymal lung changes | |||
| Parenchymal changes | All patients | PE | No PE |
| Lobes involved | |||
| 0 | 19 (16.4%) | 3 (11.5%) | 16 (18%) |
| 1 | 3 (2.6%) | 1 (3.9%) | 2 (2.2%) |
| 2 | 4 (3.4%) | 1 (3.9%) | 3 (3.4%) |
| 3 | 7 (6%) | 0 (0%) | 7 (8%) |
| 4 | 7 (6%) | 3 (11.5%) | 4 (4.4%) |
| 5 | 76 (65.5%) | 18 (69.2%) | 58 (64%) |
| Involvement of worst-affected lobe | |||
| 0 | 19 (16.4%) | 3 (11.5%) | 16 (17.8%) |
| < 25% | 33 (28.4%) | 7 (26.9%) | 26 (28.9%) |
| 25%-50% | 25 (21.6%) | 6 (23.1%) | 18 (21.1%) |
| 50%-75% | 22 (19%) | 5 (19.2%) | 17 (18.9%) |
| > 75% | 17 (14.7%) | 5 (19.2%) | 12 (13.3%) |
Death rates were higher in those patients with more extensive parenchymal involvement (p = 0.001). Nineteen patients did not have changes typical of COVID-19 on CT. CT identified a pleural effusion in four of these patients, while no patient had mediastinal adenopathy. Of the 19 patients without typical COVID-19 changes on CT, two patients died. One patient had significant underlying medical comorbidities, and the other patient developed parenchymal changes on follow-up chest radiographs.
A total of 47 patients had hilar or mediastinal adenopathy (40.5%). There was no difference in the rates of adenopathy between the PE and no PE groups. The presence of adenopathy was associated with the number of involved lobes (p = 0.001) and severity of lung parenchymal involvement (p = 0.002), but the authors found no significant association with an increased risk of ICU admission (p = 0.127) or death (p = 0.054).
More large-scale studies are now required to determine a threshold D-dimer level for undergoing CTPA in COVID-19, the researchers concluded.
Editor's note: The number of the ECR e-poster is C-15756, and you can access it via the EPOS section for the congress. AuntMinnieEurope.com's editorial team will be reporting on ECR 2021 throughout the meeting, so check our homepage regularly for further updates.