White-matter lesions linked with dementia and cognitive impairment are as common in heart failure patients as they are in those with a history of stroke, according to the latest results from a large German study presented on 2 September at the European Society of Cardiology (ESC) congress in Paris.
A group from Leipzig University Hospital has also linked the probability of white-matter lesions to the duration of heart failure. Patients with a longstanding diagnosis had more of these lesions compared with those more recently diagnosed.
"Up to 50% of older patients with heart failure have cognitive impairment, and heart failure is associated with an increased risk for dementia," noted lead author Dr. Tina Stegmann, a researcher from the Clinic and Policlinic for Cardiology. "However, it is still unclear what the pathological pathways are. Some investigators have identified changes in brain structure in patients with heart failure and cognitive dysfunction, but the findings are inconsistent."
Study goals
White-matter lesions are common structural alterations in the white matter of the brain, and their prevalence increases with age, she explained. They are associated with cerebral ischemia and cognitive dysfunction, but there are only a few reports on heart failure and white-matter lesions.
In Paris, she presented new findings from LIFE-Adult, a population-based cohort study whose 10,000 participants are between the ages of 18 and 80 and comprise a representative sample from Leipzig. All study participants underwent an extensive five- to six-hour core assessment program, including structured medical interviews, medical and psychological questionnaires, physical examination, and biological specimen collection.
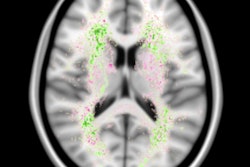
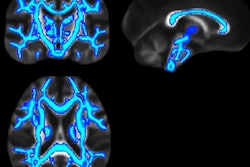
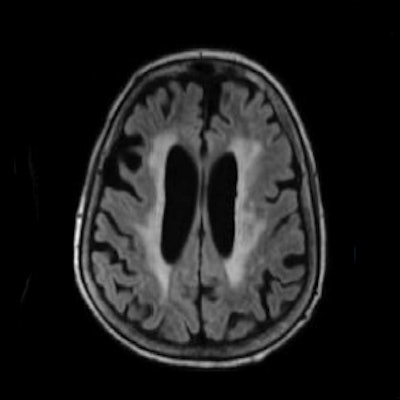
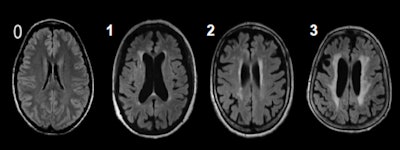 The Fazekas scale is a system for describing white-matter disease severity. It can quantify the amount of white-matter T2 hyperintense lesions attributed to chronic small vessel ischemia. Image courtesy of Dr. Tina Stegmann.
The Fazekas scale is a system for describing white-matter disease severity. It can quantify the amount of white-matter T2 hyperintense lesions attributed to chronic small vessel ischemia. Image courtesy of Dr. Tina Stegmann.A subgroup of 2,490 people additionally underwent brain MRI. Most of them had no or mild white-matter lesions (87%), and 13% had moderate or severe white-matter lesions.
The investigators sought to determine the frequency and associated risk factors for white-matter lesions in a population cohort and potentially discover a connection with heart failure. They used the Fazekas score for the classification of the white-matter lesions, and raters were blinded to other medical information of study participants. History of heart failure and other diseases were ascertained as part of the self-reported medical history questionnaire.
Main findings
The mean age of participants was 64, and 46% were women. On univariate analysis, age, troponin T, N-terminal (NT)-pro hormone BNP (NT-proBNP), body mass index, history of acute myocardial infarction, stroke, heart failure, and diabetes were positively associated with white-matter lesions, while on multivariate analysis, only age, hypertension, stroke, and heart failure were associated with white-matter lesions, Stegmann and colleagues reported.
The odds ratio for heart failure was 2.5 (95% confidence interval: 1.1; 5.6) and numerically higher than the odds ratio for stroke (odds ratio: 2.0; 95% confidence interval: 1.0; 3.8). Additionally, analysis of the duration of heart failure indicated that a long-standing diagnosis of heart failure is associated with increase of white-matter lesions (odds ratio: 1.3 for heart failure duration < 3 years; odds ratio: 1.7 for heart failure 4-6 years duration; and odds ratio: 2.9 for heart failure diagnosis > 6 years).
"Heart failure is independently associated with structural brain damage, i.e., white-matter lesions. These lesions may be a surrogate of cognitive decline and should be considered as a potential therapeutic target in heart failure," they stated.
They added that connections between heart failure, stroke, and white-matter lesions could be due to shared risk factors such as age and high blood pressure. In addition, there may be a causal link between heart failure and stroke. It is well known, for instance, that the risk of stroke is higher in patients with heart failure than without.
"The role of dementia and its prevention is of growing interest in heart failure research as the overall heart failure population is ageing and suffering from numerous comorbidities," she said. "Studies are needed to see if white-matter lesions could be a therapeutic target for treating cognitive decline in patients with heart failure. There is currently no clear indication to screen for white-matter lesions in heart failure patients using brain MRI."
Looking to the future
The patients in the subgroup will have a five-year follow-up brain MRI scan, making it possible to track the progress of the white-matter lesions, heart failure, and cognition in a longitudinal way.
"The main thing we don't know is what mechanism is behind the development of white-matter hypertensities due to cardiovascular disease," she told AuntMinnieEurope.com in an email. "Is it the overall risk profile, or are there certain pathological pathways in heart failure that lead to certain types of white-matter lesions, and how we can prevent this? Additionally, how we can prevent the development of dementia in these patients?"
The LIFE-Adult study was funded by the European Union (EU), the European Regional Development Fund (ERDF), and the Free State of Saxony.
For more details on the Fazekas scale, Stegmann recommends the following book: Mariß J, Maurer CJ. Neuroradiologische Messverfahren, Klassifikationen, und Zeichen. Stuttgart, New York: Georg Thieme Verlag; 2018.