Visualizing patient anatomy in 3D through augmented reality (AR) technology can overcome key limitations of image-guided surgery, according to researchers from Poland. They shared their initial experiences of using AR to facilitate aortic aneurysm repair in a recent article in the Journal of Endovascular Therapy.
The group from Pomeranian Medical University in Szczecin created 3D anatomical models based on the CT angiography (CTA) scans of a patient with an abdominal aortic aneurysm. Then they used AR technology to examine the 3D models and relevant imaging data during surgical treatment (J Endovasc Ther, August 2019, Vol. 26:4, pp. 544-547).
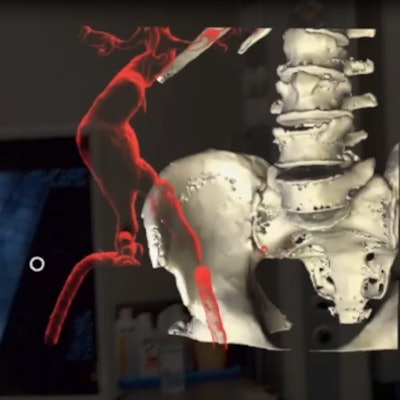
Augmented reality display of 3D models based on CT angiography scans. Video courtesy of Dr. Pawel Rynio, PhD.
This new, AR-based method allowed the surgeon to have access to the 3D CTA data directly in front of him throughout the operation and, thus, reduce his need to look away from the procedural site, lead author Dr. Pawel Rynio, PhD, and colleagues noted.
"The AR approach is most helpful, being available all the time and enabling rotation in all angles with preservation of structural relationships," they wrote. "AR systems have the potential to combine many forms of medical data, merging different screens into one shared system to keep the operator's eyes focused on the operating field."
AR for aortic repair
Using imaging technology to guide surgery is common, especially for procedures involving complex vascular anatomy. Though helpful, many current image guidance techniques are limited in their capacity to display spatial relationships in three dimensions, and often require exposing patients to radiation.
"Therefore, there is a strong need for new technologies that will be able to project a patient's anatomy with preservation of 3D relationships between structures," the authors wrote.
Several advanced visualization techniques including AR, virtual reality, and 3D printing have shown promise to that end. Among them, AR appears to be well-suited for intraoperative use because it allows clinicians to see 3D anatomical models without inhibiting their view of the operating field.
Indeed, researchers throughout Europe have demonstrated the potential advantages of incorporating AR into spinal surgery, minimally invasive procedures such as ureteroscopy, and prostate cancer removal, to list but a few examples.
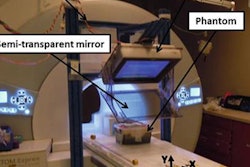
Extending this practice to vascular surgery, Rynio and colleagues used AR technology to facilitate surgical treatment for a 77-year-old patient whose CTA scans revealed a 55-mm abdominal aortic aneurysm. They used various open-source computer software (3D Slicer; Blender) to segment the scans and generate a 3D model of the patient's internal anatomy. Then they loaded the 3D imaging data into AR-compatible hologram software (Carna Life, MedApp).
A surgical team treated the patient by performing endovascular aneurysm repair -- the gold standard treatment for aortic aneurysms -- while also wearing an AR headset (HoloLens, Microsoft) to visualize transparent 3D models of the aneurysm, thrombus, and adjacent bones.
Better efficiency
The operating surgeon was able to position the 3D models at any part of the operating room using a combination of hand gestures and voice commands. He also had the option of moving, rotating, cutting, or zooming through the 3D models during surgery. For example, the surgeon could virtually detach the thrombus from the aneurysm to get a better view of either section.
In addition, the operating surgeon was able to pull up a 2D virtual display of the volume-rendered CTA scans, along with measurements of the arteries and notes from presurgical planning.
After successfully completing the aneurysm repair, the surgeon reported that AR was "useful in navigation and guidance without obscuring vision." He also stated the AR device offered good control and did not increase the risk of contamination of the operating site.
"Augmented reality with holographic imaging of CTA data is feasible and helpful during endovascular aneurysm repair," Rynio and colleagues wrote. "AR has a potential to improve perioperative outcomes; however, studies are required to assess any statistically significant impact on operating time, contrast volume, and radiation dose."
There remains room for improvement for AR guidance as well, the authors noted. The greatest limitation of AR is the quality of the 3D models relies heavily on features of the originating image, including image resolution and slice thickness. The battery life of the AR device also restricts its use to a period of two to three hours.
Regarding future advancements that could bolster the technology, the researchers cited the potential of AR to enable intraoperative visualization of a fusion of fluoroscopic data and CT-based 3D models. "Such [a] combination will potentially synergize advantages [of AR] further, reducing the contrast and radiation dose and operation time," they wrote.