In tricky cases of endometriosis, the key to success is the optimum use of MRI for preoperative staging plus multidisciplinary teamworking that encourages efficient feedback between surgeons and radiologists to ensure quality control, delegates learned at the recent Royal College of Obstetricians & Gynaecologists (RCOG) World Congress.
"MRI is really sensitive and specific for detecting endometriosis, and has such a wide field of view that we can clearly identify disease both within and beyond the pelvis, often in places that haven't been previously clinically suspected," said Dr. Susan Freeman, a consultant radiologist at Cambridge University Hospitals National Health Service (NHS) Foundation Trust in the U.K. "MRI is excellent for confirming or excluding the presence of cancer."
 MRI can help with problem-solving, says Dr. Susan Freeman.
MRI can help with problem-solving, says Dr. Susan Freeman.This chronic gynecological condition affects women of reproductive age. It may cause pelvic pain and infertility, and it is characterized by the growth of functional ectopic endometrial glands and stroma outside the uterus. The three different manifestations are ovarian endometriomas, peritoneal implants, and deep pelvic endometriosis.
Because MRI can perform a complete assessment of all pelvic compartments at one time, it is the best technique for preoperative staging of endometriosis. It can assist with preoperative evaluation of the bowel, bladder, ureters/parametria, and pelvic sidewall, as well as beyond the pelvis into the groin, perineum, and diaphragm, she explained. The modality can also help with problem-solving, e.g., in cases of indeterminate adnexal mass or raised cancer antigen 125 (CA-125) in the blood.
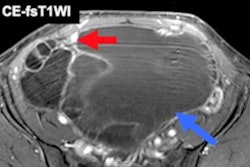
Indications of cancer in endometriosis (typically clear cell/endometrioid cancers) may include solid nodules with vascularity seen on ultrasound, as well as larger endometrioma (> 9 cm in diameter) with a soft-tissue mural nodule, loss of T2 shading, and enhancement postcontrast/restriction on diffusion-weighted imaging, Freeman told attendees at the congress, held in London from 17 to 19 June.
To improve clarity, she advocates the use of Buscopan (hyoscine-N-butylbromide) because peristalsis can ruin MR images. Also, she uses a template to report back findings to gynecologists because this helps to ensure consistency in reporting.
The primary locations are in the pelvis, but extrapelvic endometriosis does occur rarely. Around 40% of patients with invasive endometriosis have an endometrioma that is seen as a bright white lesion on T1-weighted images and as shading on T2-weighted images. Ectopic deposits of endometrium can often bleed and set up a fibrotic inflammatory response. Both fibrosis and smooth muscle appear as low signal intensity on T1- and T2-weighted imaging, and they are seen as black spiculated or solid nodules in the pelvis. Bowel endometriosis most commonly affects the rectum and rectal sigmoid, and more than half of cases have multifocal disease, Freeman added.
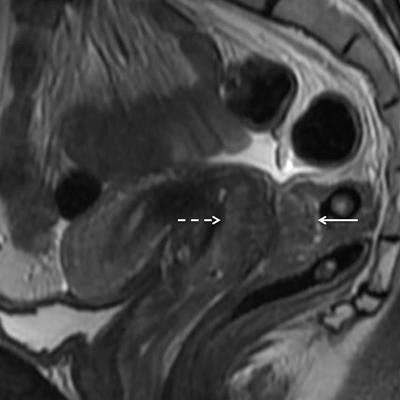
 A 34-year-old woman with dyspareunia and dyschezia. This sagittal T2-weighted image through the pelvis reveals a large endometriotic deposit within the rectovaginal septum. The mass has an "hourglass" configuration and is infiltrating the posterior vaginal fornix anteriorly (dashed arrow) and the rectal muscularis posteriorly (solid arrow). The nodule represents fibromuscular hyperplasia around ectopic endometrial glands. There is commonly preservation of the overlying rectal mucosa, seen as a high signal intensity (bright) line overlying the mass. Endometriotic infiltration of the muscle dictates a different surgical approach than the presence of adhesions or serosal involvement alone. Image courtesy of Dr. Susan Freeman.
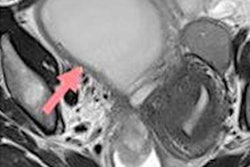
A 34-year-old woman with dyspareunia and dyschezia. This sagittal T2-weighted image through the pelvis reveals a large endometriotic deposit within the rectovaginal septum. The mass has an "hourglass" configuration and is infiltrating the posterior vaginal fornix anteriorly (dashed arrow) and the rectal muscularis posteriorly (solid arrow). The nodule represents fibromuscular hyperplasia around ectopic endometrial glands. There is commonly preservation of the overlying rectal mucosa, seen as a high signal intensity (bright) line overlying the mass. Endometriotic infiltration of the muscle dictates a different surgical approach than the presence of adhesions or serosal involvement alone. Image courtesy of Dr. Susan Freeman.Urinary tract endometriosis is quite rare, but where it does occur, it is often seen as serosal plaques and deposits on the bladder. Ureteral involvement can also arise, and this may lead to hydronephrosis. Sometimes it is difficult to see parametrial disease, but careful scrutiny may reveal medialization of the ureter, she continued.
Other places to look for endometriosis in the pelvis are cesarean scars (where it often presents as cyclical groin pain and swelling) and episiotomy scars, and very rarely it is found in the internal obturator muscle. Freeman advised delegates not to forget the nerves, because nerve pain can be an indication of endometriosis; coronal views are excellent for identifying endometriotic disease in the sciatic nerve.
4 different subtypes
The gold standard for pelvic endometriosis diagnosis is laparoscopic biopsy, but transvaginal ultrasound and MRI are the main imaging methods used for presurgical diagnosis, and to characterize and stage the disease, it is important to recognize the different signs that this disease may produce, according to Dr. Luisina Clerico and colleagues from the department of radiology, Diagnóstico Medico Oroño, Fundación Villavicencio, in Rosario, Argentina.
They classify endometriosis into four different subtypes:
- Adenomyosis is when endometrial tissue exits and grows into the muscular wall of the uterus.
- Ovarian endometriosis, also known as endometrioma, is a type of cyst formed when endometrial tissue grows in the ovary.
- Deep pelvic endometriosis is defined as invasion of endometrial glands and stroma penetrating into the retroperitoneal space or the wall of the pelvic organs to a depth of at least 5 mm.
- Extragenital endometriosis can be found in almost any tissue in the body. The endometrial tissue can exit and grow in the gastrointestinal tract, chest cavity, urinary tract, abdominal wall, and perinea. The symptoms will depend on the site of the lesions.
"Our basic protocol includes high-resolution T2-weighted sequences in all orthogonal planes as well as axial T1-weighted sequences, and axial and sagittal fat-suppressed fast spin-echo T1-weighted sequences," they stated. "When endometriosis disease was suspected, we used ultrasound gel to fill the vaginal cavity and, in some cases, we filled the rectal lumen.
Diagnosis requires a combination of clinical history and invasive and noninvasive techniques, but the definitive diagnosis is based on laparoscopy with histological confirmation. The MRI appearance of endometriotic lesions is variable and typically depends on the quantity and age of hemorrhage, the amount of endometrial cells, stroma, smooth muscle proliferation, and fibrosis. The aim of surgery is to achieve complete resection of all endometriotic lesions in the same operation.