Millions of women each year have difficulty conceiving children, a condition known as subfertility. But radiology is playing a growing role in both detecting the condition and helping to solve problems with noninvasive therapies, according to research from a leading facility in London.
"Imaging has a significant role in diagnosing the causes of subfertility and in guiding therapy," noted Dr. Saranya Vickramarajah and colleagues at Imperial College in London in an e-poster that received a certificate of merit at RSNA 2016. "Changes to the landscape of subfertility imaging include the trend in delaying motherhood, advent of newer imaging technologies, and greater uptake of in vitro fertilization."
They urged everybody to keep in mind the main points when dealing with subfertility, such as what to do for tubal pathology, and discussed techniques used directly to restore fertility, how surgical options may be aided, and pharmacological versus surgical interventions.
What is subfertility?
Subfertility is defined as the inability to conceive despite regular unprotected intercourse, and it affects around 6.7 million women in the U.S. and 3.5 million in the U.K., according to the authors. Roughly 85% to 90% of cases are treatable. Female subfertility independently contributes to one-third of all cases of infertility.
There are two main categories of female subfertility: congenital and acquired. Congenital subfertility includes the following:
- Uterine developmental anomalies and Müllerian duct anomalies
- Ovarian aplasia and hypoplasia
- Tubal structural abnormalities
- Genetic Klinefelter's syndrome and Turner's syndrome
Acquired subfertility includes the following:
- Intrauterine adhesions -- infective and noninfective
- Fibroids or polyps
- Adenomyosis and endometriosis
- Tubal disease
- Postradiation, postchemotherapy, systemic, or endocrine
Subfertility can be investigated in several ways, as shown in the table below.
| Methods for investigating subfertility | |
| Primary investigations | Secondary investigations |
| Assess ovulation; serum progesterone, luteinizing hormones/follicle-stimulating hormone levels | Ovarian reserve assessment |
| Hormone testing | Genetic testing |
| Prolactin | Transabdominal/transvaginal ultrasound |
| Thyroid test | Laparoscopy |
| Androgen profile | Hysterosalpingography |
Imaging's role
Imaging of subfertility can be performed in several ways, and Vickramarajah and colleagues advocated a multimodality approach to diagnose structural abnormalities.
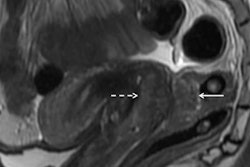
Ultrasound, either transabdominal or transvaginal, is highly operator-dependent. Fluoroscopic hysterosalpingography is also operator-dependent, but in diagnostic use it offers dynamic assessment of the uterine cavity and fallopian tubes. In therapeutic use, it offers selective tubal catheterization and/or tubal recanalization.
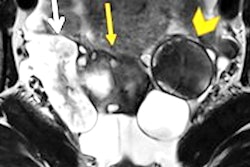
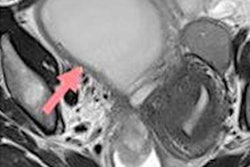
MRI can help further clarify and characterize abnormalities such as Müllerian duct anomalies, and it should be a second-line or adjunctive investigation to ultrasound in assessing fibroid disease and deep pelvic endometriosis, the authors stated.
"These approaches are long-established and continue to be adapted," they wrote. "Of more interest are the implications for imaging in the treatment and restoration of fertility."
Types of subfertility
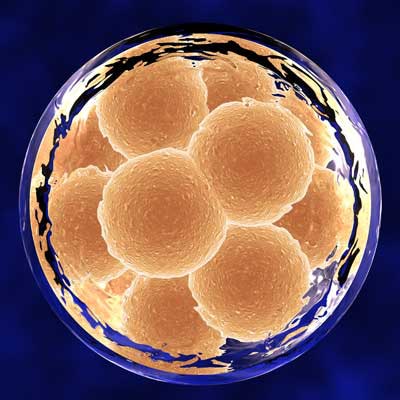
In their RSNA e-poster, Vickramarajah and colleagues outlined several kinds of subfertility. One example is polycystic ovarian syndrome (PCOS), a diagnosis based on a combination of clinical, biochemical, and ultrasound findings. A woman with PCOS must have two of the following three criteria:
- Chemical and/or biochemical hyperandrogenism
- Oligomenorrhea or oligo-ovulation
- Polycystic ovaries on ultrasound
Polycystic ovarian morphology consists of more than 12 cysts with diameters of 2 mm to 9 mm and/or increased ovarian volume (> 10 mL).
Ultrasound is important but not adequate to diagnose PCOS alone. Also, the authors cautioned that multifollicular ovaries can be mistaken for PCOS. The differences include the following:
- Ovaries are normal around menarche.
- Ovaries are small volume with several small follicles.
- Uterus is small with a thin endometrium.
- Associated with weight loss, anorexia nervosa, and low estrogen levels.
Another type of subfertility is tubal pathology, which is the cause of subfertility in 25% to 35% of subfertile couples. Hysterosalpingo-contrast-sonography is a noninvasive way without ionizing resradiation to assess the cavity and tubal patency. The technique uses endovaginal ultrasound with simultaneous transcervical injection of ultrasound contrast agents or saline. It's performed during the midproliferative phase (days 6 to 10). The initial transvaginal ultrasound scan is carried out to assess the position of pelvic organs and rule out any pathology that would come in the way of the procedure. The reported sensitivity is 93.3%, and the specificity is 89.7% among experienced practitioners.
Other treatments for subfertility include the following:
- Fallopian tube recanalization
- Endometrioma drainage
- MR-guided focused ultrasound or myomectomy for fibroids
Also, imaging can help plan fertility optimization/restoration in benign disease, including the following:
- Endometriosis: surgical road map in deep pelvic endometriosis
- Planning and monitoring adhesionolysis in Asherman's
- Müllerian duct anomalies: delineate anomaly to guide management
- Imaging evaluation prior to uterine transplantation
"The full range of congenital anomalies which may impact on fertility is vast and beyond our remit," the authors concluded, although some of the more common cases were presented in their e-poster.