MRI has an essential role in the preoperative assessment of candidates for fertility-sparing treatment in women with gynecological malignancies, Spanish researchers have reiterated. Appropriate patient selection based on tumor staging is paramount, they emphasize.
It's important for radiologists to know the current options of fertility-sparing treatment for the most common gynecologic cancers, according to Dr. Natalie Antunes, Dr. Carlos Nicolau, and colleagues in the radiology department at Hospital Clinic Barcelona. They urge everybody to understand the current eligibility criteria for fertility-sparing treatment -- especially the imaging-dependent ones -- and to be aware of the standard imaging report of each gynecological malignancy to address such selection criteria.
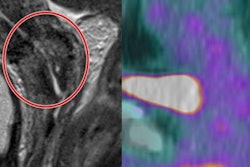
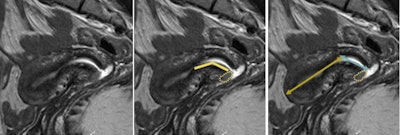 Sagittal T2-weighted MR images in a 35-year-old woman with confirmed adenocarcinoma of the cervix show anterior lip tumor (yellow dotted lines). The distance from the proximal aspect of the tumor to the internal os is marked (yellow lines), to allow for at least 1 cm of healthy cervical stroma between the internal os and the future surgical anastomosis. This will reduce the risk of ascending infection, cervical incompetence, and premature delivery. The length of the uterine corpus (yellow/brown arrow) and cervix (blue arrow) should also be included in the imaging report of possible FST candidates. All figures courtesy of Dr. Natalie Antunes and Dr. Carlos Nicolau and RSNA 2020.
Sagittal T2-weighted MR images in a 35-year-old woman with confirmed adenocarcinoma of the cervix show anterior lip tumor (yellow dotted lines). The distance from the proximal aspect of the tumor to the internal os is marked (yellow lines), to allow for at least 1 cm of healthy cervical stroma between the internal os and the future surgical anastomosis. This will reduce the risk of ascending infection, cervical incompetence, and premature delivery. The length of the uterine corpus (yellow/brown arrow) and cervix (blue arrow) should also be included in the imaging report of possible FST candidates. All figures courtesy of Dr. Natalie Antunes and Dr. Carlos Nicolau and RSNA 2020.Gynecological malignancies are among the leading causes of cancer-related morbidity and mortality worldwide. The three most common -- cervical, endometrial, and ovarian -- accounted for around 14% of diagnosed female cancers in 2018, and about 20% of these patients are under the age of 40.
The adoption of large-scale screening strategies and development of modern surgical and nonsurgical therapies have improved the early-stage diagnosis and treatment of these tumors. What's more, the improved survival rates and tendency to delay childbearing have made fertility preservation options valuable for the affected women, contributing to the emergence of oncofertility, the group explained in an RSNA 2020 e-poster for which they received a certificate of merit.
Criteria for fertility-sparing therapy
Cervical cancer is the fourth most common cause of cancer and cancer-related mortality in women, and 43% of diagnosed patients are under the age of 45, the team continued. The following are the eligibility criteria for cervical carcinoma fertility-sparing treatment:
- Confirmed squamous cell carcinoma, adenocarcinoma, or adenosquamous histology
- Federation of Gynecology and Obstetrics (FIGO) stage IA1, IA2, and IB1 (IB2 in selected cases)
- Tumor diameter ≤ 2 cm (≤ 4 cm in some centers if exophytic tumor)
- Tumor-to-internal os distance ≥ 1 cm
- Depth of stromal invasion < 50%
- Absence of parametrial invasion and lymph node metastasis
Endometrial cancer is the most common gynecological cancer in developed countries. Typically, it occurs in postmenopausal women, but around 7% of cases are found in women under 45. The main risk factor is unopposed estrogen exposure, for example in women with obesity and polycystic ovary syndrome.
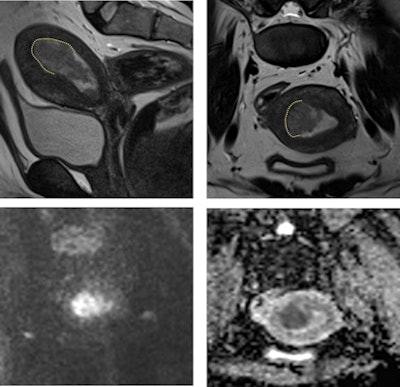 Sagittal (top left) and axial (top right) T2-weighted, diffusion-weighted (b1000 sec/mm2; bottom left), and apparent diffusion coefficient map (bottom right) MR images in an 18-year-old patient with confirmed endometrial intraepithelial neoplasia. MRI is critical to confirm eligibility for FST by excluding myometrial invasion, as in this case (dotted line).
Sagittal (top left) and axial (top right) T2-weighted, diffusion-weighted (b1000 sec/mm2; bottom left), and apparent diffusion coefficient map (bottom right) MR images in an 18-year-old patient with confirmed endometrial intraepithelial neoplasia. MRI is critical to confirm eligibility for FST by excluding myometrial invasion, as in this case (dotted line).MRI is paramount in excluding myometrial invasion and tumor extension beyond the uterine corpus, according to the authors, who noted that the eligibility criteria for endometrial carcinoma fertility-sparing treatment are the following:
- Well-differentiated (FIGO stage 1) endometrioid adenocarcinoma or premalignant conditions such as atypical hyperplasia or endometrial intraepithelial neoplasia
- No contraindications to progestins, no evidence of myometrial invasion on MRI, and no evidence of extrauterine disease on staging with CT or MRI
- Absence of lymph node metastasis, and absence of synchronous primary ovarian cancer or ovarian metastases
"Ovarian cancer is the most lethal tumor among gynecological cancers," Antunes, Nicolau and colleagues pointed out. "The lack of screening programs, early symptoms, and sensible tumor markers contribute to the usual high grade of diagnosis at late stages."
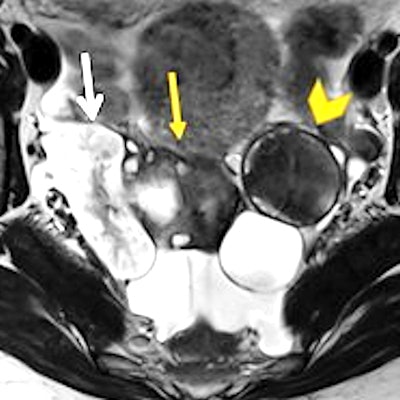
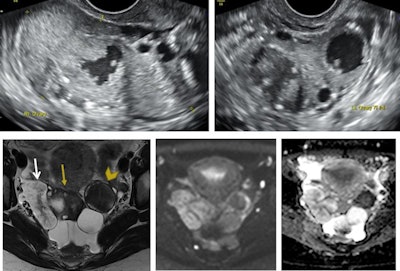 Transvaginal ultrasound images of the right ovary (top left image) and left ovary (top right image) in a 31-year-old nulliparous patient. Both ovaries are enlarged and heterogeneous with solid and cystic areas. Follow-up MRI with axial T2-weighting (bottom left image), diffusion-weighting (b1000 sec/mm2; middle image), and apparent diffusion coefficient map (bottom right image) show right ovary (yellow arrow) with adjacent solid tissue (white arrow) and abnormal left ovary (yellow arrowhead). Operative findings reported a 5 cm cluster of papillary tissue protruding from the right and left ovaries with two cysts. Perioperative biopsy confirmed bilateral borderline serous ovarian tumor and bilateral salpingo-oophorectomy was performed, associated with infracolic omentectomy and peritoneal biopsies.
Transvaginal ultrasound images of the right ovary (top left image) and left ovary (top right image) in a 31-year-old nulliparous patient. Both ovaries are enlarged and heterogeneous with solid and cystic areas. Follow-up MRI with axial T2-weighting (bottom left image), diffusion-weighting (b1000 sec/mm2; middle image), and apparent diffusion coefficient map (bottom right image) show right ovary (yellow arrow) with adjacent solid tissue (white arrow) and abnormal left ovary (yellow arrowhead). Operative findings reported a 5 cm cluster of papillary tissue protruding from the right and left ovaries with two cysts. Perioperative biopsy confirmed bilateral borderline serous ovarian tumor and bilateral salpingo-oophorectomy was performed, associated with infracolic omentectomy and peritoneal biopsies.Most ovarian malignancies present in postmenopausal patients, but most found in women of reproductive age are germ-cell tumors or epithelial borderline tumors. In the case of epithelial ovarian cancers, about 14% of all cases occur in women under 40.
The eligibility criteria for ovarian carcinoma fertility-sparing treatment are the following:
- Malignant germ-cell tumors, malignant sex-cord stromal tumors, borderline ovarian tumors, and epithelial ovarian cancers (stage IA and unilateral inferior colliculus)
- No evidence of contralateral ovary involvement, and no evidence of pelvic or peritoneal extension
- Absence of lymph-node metastasis, and absence of distant metastasis
The Barcelona team is now working on projects concerning the value of diffusion in endometrial cancer and the usefulness of MRI in cervical cancer patients treated with radiation therapy, but its work is being affected greatly by the pandemic.
"COVID-19 has impacted not only the follow-up of gynecological malignancies -- as patients present later to scheduled controls owing to the fear of transmission -- but also their diagnosis and treatment, as there are less available operating rooms in a hospital. Staff are under strain and numbers are depleted due to COVID-19 care," Antunes told AuntMinnieEurope.com.