Belgian researchers said they have achieved remarkable reductions in costs, radiation dose, and -- most important -- negative angiography studies by implementing fractional flow reserve CT (FFR-CT) to manage the care of patients with chest pain who have an intermediate risk of coronary disease. If validated in larger studies, the results could transform the care of these patients to make it cheaper, safer, and more effective, they said.
 Dr. Johan De Mey from Universitair Zuikenhaus Brussel.
Dr. Johan De Mey from Universitair Zuikenhaus Brussel.The group retrospectively examined results in 48 stable patients with chest pain who had a positive exercise ECG test and intermediate stenosis of 50% to 70% on coronary CT angiography (CCTA) and were referred for invasive coronary angiography and invasive fractional flow reserve. They sought to assess the impact of adopting noninvasive FFR-CT to guide clinical decision-making in these patients. The investigators from Vrije University and University Hospital in Brussels found that FFR-CT could reduce the number of unnecessary catheterizations by 80%, while also cutting risks of morbidity and mortality and costs.
"This new method could become the gateway to the cath lab, and in this way make it much safer for the patients while reducing costs," said study co-author Johann De Mey, who presented the results on behalf of lead investigator Dr. Kristof De Smet at the RSNA 2016 meeting in Chicago.
Costly care
Caring for patients with chest pain is one of the riskiest and most expensive indications in modern medicine, generating as much as $6 billion U.S. (5.66 billion euros) in annual costs in the U.S. alone for patients presenting to emergency departments. But for all the money spent, outcomes fall far short of where they could be, according to De May.
"Fifty-five percent of patients coming from noninvasive functional testing and going to the cath lab have no need for [percutaneous coronary intervention] or [coronary artery bypass graft [CABG], and we'd like to have a better test for sending patients to the cath lab," De Mey said of a 2014 paper by Cury et al. "Maybe CT can offer us a solution."
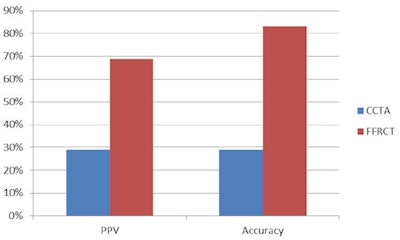 FFR-CT had higher diagnostic accuracy than CCTA (83% versus 29%) with higher positive predictive value (69% versus 29%). All images courtesy of Dr. Kristof De Smet.
FFR-CT had higher diagnostic accuracy than CCTA (83% versus 29%) with higher positive predictive value (69% versus 29%). All images courtesy of Dr. Kristof De Smet.CCTA is a great tool for evaluating young patients with chest pain and for those with a low and intermediate risk of heart disease, but by itself it is inadequate for confirming obstructive coronary disease that requires intervention, he said. And even though CCTA results correlate well with angiography with regard to stenosis severity, CT cannot reliably estimate the hemodynamic significance of lesions.
CT is "not that good if we underestimate the hemodynamic significance of lesions as determined by fractional flow reserve during invasive procedures," De Mey said. Most coronary artery lesions of even 50% luminal narrowing and more at CT have no hemodynamic significance, and 75% of patients referred with a positive CT result do not have significant lesions, he said.
Noninvasive FFR-CT could determine the hemodynamic significance of coronary artery stenosis based on computation of fluid dynamics, De Mey said.
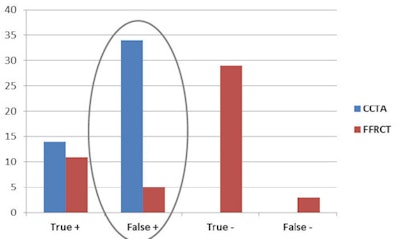 FFR-CT adoption produced a sixfold reduction of false positives.
FFR-CT adoption produced a sixfold reduction of false positives."It takes into account the morphology from the coronary tree, takes into account the muscle of the heart, and then based on fluid dynamics gives us a number, a quantification for each part of the coronary tree. Any result below 0.8 for a vessel means there's a problem and the patient requires revascularization.
"The purpose of our study is to investigate whether FFR-CT images and data could reduce costs, risks, and radiation exposure in symptomatic patients with lesions of 50% or greater on CT by reducing the number of unnecessary patients in the cath lab," De Mey said.
False positives plummet
The 48 patients in the study all had stable chest pain, a positive exercise ECG, and intermediate CCTA stenosis of 50% to 70%. All were referred for invasive angiography and invasive FFR evaluation. The study included blinded FFR-CT analysis by FFR-CT provider Heartflow to determine the diagnostic accuracy of FFR-CT versus CCTA using FFR as a reference standard.
The results showed that FFR-CT had 83% diagnostic accuracy versus 29% for CCTA, with a higher positive predictive value of 69% versus 29% and a sixfold reduction in false positives, from 34 with CCTA to five with FFR-CT.
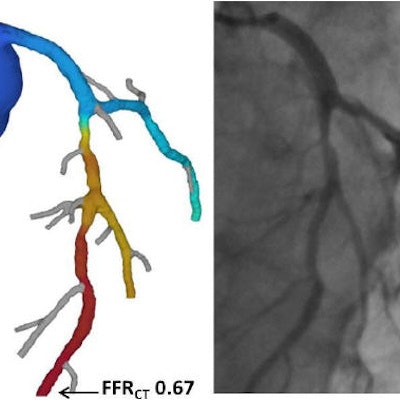
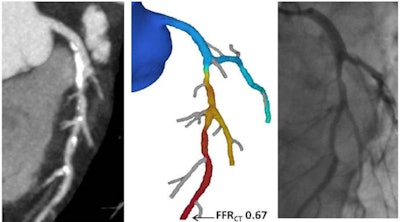 Fractional flow result of 0.67 (center) based on computational fluid dynamics reveals hemodynamically significant lesions requiring revascularization.
Fractional flow result of 0.67 (center) based on computational fluid dynamics reveals hemodynamically significant lesions requiring revascularization.Moreover, noninvasive FFR-guided therapy revealed that 71% of patients (34 of 48) had nonobstructive coronary disease (FFR > 0.8) and could be treated medically. Another 14 patients (29%, 14 of 48) had FFR of 0.8 or lower and underwent revascularization -- eight with percutaneous coronary intervention (PCI) and six with coronary artery bypass grafts (CABG). No adverse events were recorded.
Using FFR-CT, the number of unnecessary angiography and invasive FFR procedures fell by 85%, with immediate reductions in the inherent risks of an invasive procedure, including bleeding, arrhythmia, stroke, dissection, myocardial infarction, and more.
"Assuming a cost of FFR-CT of about 1,000 euros, use of the technique would have cut costs in Belgium by about 30% -- and the savings tend to be higher if you take into account the cost of those invasive procedures," De Mey said.
Finally, radiation exposure would fall by 63% if you assume a dose of about 2.5 mSv for CCTA and 4.8 mSv for catheterization, he said, noting that radiation doses continue to fall for both procedures. FFR-CT could become the gateway for the cath lab, with multiple benefits for patients, and reduced costs of care, he said, noting that larger studies are needed to validate these results.
For example, FFR-CT still produced three false negatives, maybe a cutoff of 0.85 rather than 0.8 would take care of this issue, De Mey said.
In response to a question from a session moderator, De Mey said that chances of reimbursement for FFR-CT and widespread clinical implantation may depend on political as well as clinical factors.
"At this moment I think it will not be reimbursed because there's not enough money -- I think all over the world -- so we will have to fight for it," De Mey said. "In my opinion, if you calculate the cost of invasive angio, hospitalizations ... and if you can get some of that money and shift it to FFR-CT, I think it would benefit patients and health. But in Belgium, invasive angiography is done by the cardiologist, and CT scans are done by the radiologist, so we have to shift money from cardiology to radiology -- and from radiology to the [FFR-CT] companies. I think this is the most difficult problem to tackle, so we need more evidence and time to prove to the governments that it's working."