
LONDON - A leading cardiologist's perspective on the current clinical controversies surrounding coronary CT angiography (CCTA), as provided by Dr. Stephan Achenbach, professor and chairman of the department of cardiology at the University of Erlangen in Germany, was the main crowd-puller at last week's annual conference of the British Institute of Radiology (BIR).
In his keynote lecture, Achenbach addressed an ongoing debate over the use of CT in cardiac applications, explaining the pros and cons of using the modality to visualize the coronary arteries, and its potential role in identifying stenoses that cause ischemia.
He acknowledged that CT was becoming an increasingly important diagnostic tool in cardiology, mainly because of its effectiveness in visualizing the coronary arteries and identifying stenoses in patients with acute or stable chest pain. But many patients have nothing wrong with their coronary arteries and still have chest pain, he pointed out.
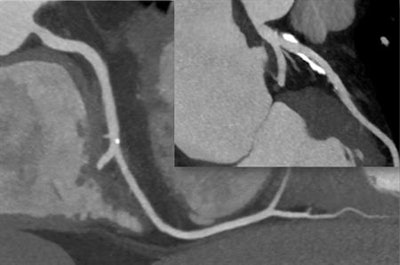 CT scan shows two separate coronary arteries without stenosis or narrowing. There is calcification, and if CT is not performed well (high motion, low-quality image), these calcifications can cause false-positive findings. Image courtesy of Dr. Stephan Achenbach.
CT scan shows two separate coronary arteries without stenosis or narrowing. There is calcification, and if CT is not performed well (high motion, low-quality image), these calcifications can cause false-positive findings. Image courtesy of Dr. Stephan Achenbach."CT is particularly good at identifying those patients without stenosis who do not require further work-up. Effectively, showing that the coronary arteries are normal is the main value of CT," he said.
Achenbach noted the use of CT for this purpose was growing, and that, more and more, the guidelines were reflecting this, adding there were also a few other applications, e.g., when a coronary artery is completely occluded, where CT can aid intervention.
"But its value in this context is relatively small compared with its role in patients with chest pain," he continued.
Image quality is key in CCTA
Turning to the continuing debate on the use of CT in cardiology, Achenbach highlighted that people fell into one of two camps: those markedly in favor and those who were huge opponents.
He stressed that by understanding the reasons for resistance, we can be better able to improve the situation. Highlighting the risk of false-positive results if CT is performed at poor image quality, Achenbach noted a patient whose scan generates a poor-quality CT might consequently undergo a substantial amount of downstream testing, which is unnecessary. Because CT is being used in a low-risk population generally, then it's vital to ensure the specificity is high, he said.
A typical false positive might arise where a patient actually has atherosclerosis on CT with calcifications, Achenbach explained. It might be interpreted as stenosis due to a poor-quality image.
"This is not good for the patient because they have some plaque but no stenosis," he noted. "However, using high-end technology and ensuring that the scan is acquired correctly can ensure in these difficult situations we can confidently rule out stenosis."
Achenbach added that to obtain the best quality of image possible, it was necessary to lower the heart rate and ensure contrast is good. Together, these should minimize the number of false positives.
Stenoses that cause ischemia
However, Achenbach asserted the importance of determining whether a stenosis is causing ischemia and has hemodynamic relevance before progressing to revascularization. A shift in opinion concerning when to surgically remove a stenosis has occurred over recent years. In the past, if a stenosis or any narrowing was seen, then it was considered best to remove it, but recently it has become clear that not every stenosis causes ischemia.
"It is only useful to remove a stenosis if it causes ischemia, so beyond identifying stenosis [with CTA] it is necessary to demonstrate ischemia," he commented, adding with the way CT is currently performed, it can only show the presence or absence of stenosis. "This is good, but if you find a stenosis on CT, then the cardiologist's job is not done. We need to find out if this stenosis is causing ischemia."
 Dr. Stephen Achenbach. Image courtesy of the European Society of Cardiology.
Dr. Stephen Achenbach. Image courtesy of the European Society of Cardiology.In this respect, the patient can either undergo another test or technology can find a way to improve the identification of ischemia with CT. This is something researchers are working on right now, Achenbach remarked.
Perfusion may be one way of acquiring information on whether the stenosis is causing ischemia. An alternative is fractional flow reserve (FFR) computed from noninvasive CT angiography (FFRCT), which is essentially a computer-modelling system that simulates and calculates whether the presented anatomy precipitates ischemia. This has still not fully penetrated into clinical application, but eventually could reduce the need for invasive coronary angiography. FFRCT is promising, according to Achenbach, but currently produces accuracies of 85%.
"This is very good but is this enough clinically? With a 15% chance of uncertainty, some are afraid that we might miss something, which is why this has not been taken up clinically to a large degree yet," he said.
Overall, Achenbach highlighted CT was already an extremely valuable tool in the diagnosis of coronary artery disease but there were some limitations that looked likely to be overcome in the near future.
"CT is very useful to rule out stenosis, but it needs to be done well and if a stenosis is found then the job is not done, you need to know if that stenosis causes ischemia or not."



















