Next August's annual congress of the European Society of Cardiology (ESC) is to be held virtually, not face-to-face in London, ESC President Prof. Dr. Stephan Achenbach has confirmed. In an exclusive interview, he reveals why the ESC made this decision so early and shares his views on CT's role in COVID-19 cases, collaboration with radiology, and the work of his research team.
Achenbach is chairman of cardiology and a professor of medicine at the University of Erlangen, Germany, and he became ESC president in September 2020. He won the 2017 Minnie award for Most Influential Radiology Researcher. His research interests focus on cardiovascular imaging, mainly CT, for the early detection and characterization of coronary atherosclerosis, and for the support of coronary and cardiovascular interventional procedures.
Q: Will the ESC Congress 2021 be online-only? If so, why did you decide this now?
 Prof. Dr. Stephan Achenbach. Photo courtesy of Leonard Billecke.
Prof. Dr. Stephan Achenbach. Photo courtesy of Leonard Billecke.A: Yes, this is correct. It was a difficult decision, but here is the reasoning behind it: A lot of planning goes into an ESC Congress. Planning starts, usually, far more than a year before the actual congress ever happens. But online events are completely different from onsite events. Formats, program, content ... everything needs to be different. So a "last-minute switch" from what was originally planned as an onsite event to an online format will deliver suboptimal results.
Hence, the ESC Board made a bold decision -- with the prospects for COVID-19 in 2021, let's give ourselves the room to put all our resources into planning the optimal online event. This is made possible by the early decision to go digital in 2021.
There is also the consideration that in the healthcare environment, we have a special responsibility to not spread the virus. And a global congress is a very problematic event in this regard. Awareness of that special responsibility also helped us to confidently make that decision.
Q: Will you reconsider your decision if it's deemed safe to stage a face-to-face meeting next year?
A: Even if it were deemed "safe" to have an onsite event in London in the summer of 2021, the circumstances would not let us have the big, global event that ESC Congress has come to be known for.
Q: How many CT and MRI exams do you perform in your department each year?
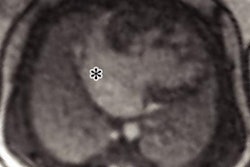
A: We perform about 1,500 cardiac CT scans with a dual-source CT system annually and about 700 cardiac MRI studies, the latter in cooperation with our radiologists.
Q: During the pandemic, what lessons have you learned about the optimum use of CT?
A: The pandemic -- at least in my institution -- has not changed the use of cardiac CT very much. Luckily, we have been able to pretty much uphold our volume of patients and also of our interventional cardiology procedures.
 High-grade stenosis of the left anterior descending coronary artery in 3D reconstructed and 2D coronary CT angiography. All clinical images courtesy of Prof. Dr. Stephan Achenbach.
High-grade stenosis of the left anterior descending coronary artery in 3D reconstructed and 2D coronary CT angiography. All clinical images courtesy of Prof. Dr. Stephan Achenbach.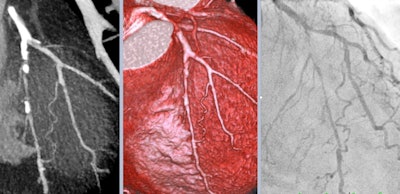 Comparison of the spatial resolution of coronary CT angiography and invasive coronary angiography: long, subtotal left anterior descending coronary artery stenosis with a collateral from the diagonal branch.
Comparison of the spatial resolution of coronary CT angiography and invasive coronary angiography: long, subtotal left anterior descending coronary artery stenosis with a collateral from the diagonal branch.The option to rapidly rule out coronary artery disease (CAD) in patients with low-risk acute chest pain by CT is a very attractive one, though, and it is used more than before. This is done with the aim to discharge patients immediately from the emergency room and avoid having to admit them to the wards.
Q: What do you see as CT's role in COVID-19 cases? How many patients have you seen with the disease?
A: We currently have about 25 patients with the disease in our hospital, which is relatively low. During the first wave, one of my department's cardiology wards had been converted to an isolation area, and I saw quite a few COVID-19 patients. Many of them were in a condition where the further course seemed rather difficult to predict for a while, but then they improved very suddenly.
There was an initial drive by some to suggest that a chest CT would be the best "first test" for suspected cases of COVID-19. We and others see a lot of CT imaging changes that might be due to COVID-19 but then turn out not to be related to it. This has a lot to do with the pretest likelihood and prevalence of COVID-19 in the population. More importantly, the polymerase chain reaction tests have become faster and much more available, which has reduced the role as a preferred initial test that CT had taken in some of the most severely affected regions.
For cardiac CT in patients with COVID-19, if the pretest likelihood of CAD is high, I am not a big fan. Such patients may then end up needing two tests -- a CT first and then invasive angiography. Then two teams will have patient contact with infection risks. So once again it depends a lot on pretest likelihood.
Q: Which aspects of cardiac imaging excite you most at present?
A: As before, we are working on the relationship between cardiac imaging and cardiac intervention. This is what excites me most at this point in time.
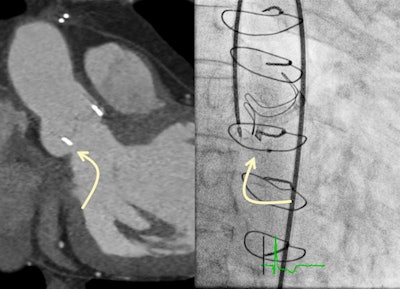 Paravalvular leak of an aortic valve bioprosthesis. In CT angiography, size and location of the leak as well as the optimal projection for fluoroscopic visualization can be determined (left). Right: interventional closure.
Paravalvular leak of an aortic valve bioprosthesis. In CT angiography, size and location of the leak as well as the optimal projection for fluoroscopic visualization can be determined (left). Right: interventional closure.Imaging is superbly important to permit and to move ahead all the new structural heart interventions.
Q: You have always been a keen supporter of collaboration between radiology and cardiology. What is your philosophy in this area?
A: We need to focus on quality, and focus on the issue. Educational activities should be open to everyone. We can learn a lot from each other, so let's do it.
Science is greater than segmentation by subspecialties. In the end, it is about the patient; in our area of work we need knowledge from both sides, and it does not really matter which side we are approaching the patient from.
Q: Have you spoken with ESR President Prof. Dr. Michael Fuchsjäger since you became ESC president? Do you plan to have regular contact with him?
A: The pandemic and its consequences have taken up most of my time so far. But I will certainly speak with Prof. Dr. Fuchsjäger and hope to be able to go to Vienna for a meeting at some point.
Q: How has the pandemic affected your daily routine?
A: My workdays have been affected very little. I am lucky to be able to go to work normally, even though the work and interaction inside the hospital have changed a lot, of course.
 Building a relationship with patients is more difficult now, Achenbach says. Photo courtesy of the European Heart Journal.
Building a relationship with patients is more difficult now, Achenbach says. Photo courtesy of the European Heart Journal.Facemasks are natural now, face-to-face meetings and courses do not take place, there is no traveling, and handshakes are gone -- establishing a good relationship with my patients has become a bit more difficult now.