Concurrent with its annual meeting this week in London, the European Society of Cardiology (ESC) has published new guidelines for diagnosing infective endocarditis (IE) in the European Heart Journal. For the first time, the guidelines emphasize the importance of multimodality imaging in endocarditis diagnosis and management.
In a recent study, the multimodality approach dramatically reduced one-year mortality in patients with infective endocarditis, from 18.5% to 8.2%. Beyond multimodality imaging, patient management by an endocarditis team is considered to be one of the most important new recommendations, according to Dr. Gilbert Habib, chairperson of the guidelines task force, in a statement.
Major changes from 2009
"While the 2009 guidelines focused on echocardiography, the 2015 guidelines show the important role of other imaging techniques such as PET/CT," Habib said. "These new imaging techniques are increasingly useful for the diagnosis and management of infective endocarditis, and we recommend their use in a novel ESC diagnostic algorithm."
The guidelines offer recommendations for the combination of early diagnosis, early antibiotic therapy, and early surgery. Regarding antibiotic prophylaxis, the 2009 guidelines recommended antibiotics only for patients at the highest risk of infective endocarditis undergoing the highest-risk dental procedures.
Yet despite increasing incidence of endocarditis thought to be related to such procedures, the 2015 guidelines did not expand the recommendations for antibiotic prophylaxis, because the ESC's committee for practice guidelines believes that the literature remains inconclusive on the subject. Instead, the 2015 guidelines focus on prevention rather than prophylaxis to prevent new cases, particularly in hospital-acquired endocarditis, the ESC wrote (Eur Heart J, 29 August 2015).
"Mortality can be reduced by multidisciplinary management in endocarditis centers. And we urge physicians to send patients with infective endocarditis for early surgical assessment as soon as possible," the ESC concluded in its statement.
The ESC urges health professionals to take the new guidelines fully into account when exercising their clinical judgment, but the guidelines are not intended to override health professionals' individual responsibility to make appropriate decisions in each individual case, the society wrote.
2015 guidelines
Despite recent improvements in management, infective endocarditis remains a deadly disease that is associated with high mortality and severe complications, the guidelines authors wrote. The 2009 guidelines introduced important concepts such as antibiotic prophylaxis for the riskiest patients, a focus on hospital-acquired infective endocarditis, and identifying the best timing for surgical intervention.
The new guidelines recognize the need for a collaborative approach among primary care physicians, cardiologists, surgeons, microbiologists, infectious disease specialists, and other physicians. The main objective is to provide clear and concise recommendations for diagnosis and care based on currently available literature. An evidence-based scoring system was used to rank the strength of recommendations, the ESC committee wrote.
Prevention via antibiotic prophylaxis was based on observational studies and animal models aiming to "prevent the attachment of bacteria onto the myocardium after transient bacteremia" following a wide range of invasive procedures, the authors wrote.
Low-grade bacteremia occurs during daily routine activities such as toothbrushing, flossing, or chewing, especially in patients with poor dental health, the group wrote. The estimated risk of infective endocarditis following dental procedures is low, estimated at one case per 150,000 dental procedures.
Moreover, the widespread use of antibiotics carries a small risk of anaphylaxis and potentially a bigger risk of widespread antibiotic resistance. Owing to these risks, antibiotic prophylaxis has been restricted to patients at highest risk of endocarditis or those with the risk of the worse outcomes.
The 2008 National Institute for Health and Care Excellence (NICE) guidelines went so far as to advise against any antibiotic prophylaxis for dental and nondental procedures regardless of patient risk, the authors wrote. The results of four studies have been mixed on the whole, but most have estimated a low risk of infective endocarditis from procedures.
Patients at risk
The patients at highest risk of infective endocarditis can be divided into three categories:
- Patients with a prosthetic valve or prosthetic material used for cardiac valve repair are at high risk.
- Patients with previous infective endocarditis also have a greater risk of new cases, as well as higher mortality and a higher incidence of complications than patients with native valves.
- Patients with transcatheter-implanted prostheses and homografts also are thought to share these higher risks.
Guidelines from the American Heart Association and American College of Cardiology recommend prophylaxis for cardiac transplant recipients who develop cardiac valvulopathy, but the ESC task force does not recommend this measure, considering the supporting evidence weak, the ESC authors wrote.
The guidelines recommend strict dental and cutaneous hygiene, disinfection of wounds, eradication of bacteria, and no self-medication with antibiotics. Piercing and tattooing should be discouraged, and the use of infusion catheters and invasive procedures should be limited as much as possible, the group recommended.
Risky procedures include high-risk dental procedures, respiratory tract procedures, gastrointestinal or urogenital procedures, and skin and soft-tissue procedures.
Imaging techniques
Echocardiography plays a key role in the diagnosis and management of infective endocarditis, as well as the prognostic assessment of patients with the condition, the authors wrote.
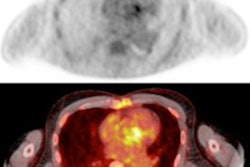
The risks of vegetation embolization or hemodynamic decompensation during coronary angiography have led to proposals for the use of multidetector-row CT (MDCT) angiography as an alternative technique. MDCT can detect abscesses and pseudoaneurysms with high diagnostic accuracy, and it is potentially better than echocardiography for delineating the extent and prognosis of perivalvular extensions, pseudoaneurysm, and abscesses. Modalities such as MRI, FDG-PET/CT, and other functional imaging modalities also have a role in endocarditis diagnosis and management, the team wrote.
In particular, MRI's high soft-tissue contrast can be helpful, although CT may be faster and more practical to administer in very ill patients, and it carries a lower contrast burden than MRI, the authors wrote.
"Systematic cerebral MRI has an impact on the diagnosis of IE since it adds one minor Duke criterion in patients who have cerebral lesions and no neurological symptoms," the authors wrote. In one study, cerebral MRI findings upgraded the IE diagnosis in 25% of patients presenting initially with nondefinite IE. Cerebral microbleeds are detectable with a 7-tesla MRI scanner.
Several studies have shown positive results from SPECT/CT and PET/CT, the guideline authors wrote.
"The main added value of using these techniques is the reduction in the rate of misdiagnosed IE, classified in the 'possible IE' category using the Duke criteria, and the detection of peripheral embolic and metastatic infectious events," the writing group noted.
Limitations include poor localization of septic emboli in the brain due to high tracer uptake in the cortex, and the fact that metastatic infections are generally smaller than 5 mm in diameter, beyond the spatial resolution thresholds of current PET/CT scanners.