"Radiation oncology and technological innovation: A fish desperately looking for a bicycle?" This was the intriguing title put forward by Dirk Verellen, PhD, for his Breur Award Lecture at the 3rd European Society for Radiotherapy and Oncology (ESTRO) Forum, held in Barcelona, Spain, in late April.
The Breur Award, the highest accolade that can be bestowed on an ESTRO member, recognizes the major contribution made by the winner to European radiotherapy. Verellen, head of medical physics at UZ Brussel in Belgium, took the opportunity to examine whether high-tech solutions are really making a difference or just looking for problems to solve.
No one can argue that technological developments have not made a huge impact upon the practice of radiation oncology, Verellen said, and research in this field must continue. However, it's important that developments are not just introduced for the sake of perceived, but not always necessary, clinical needs. "New technology should adapt to the user, not force the user to adapt to the new technology," he said, citing George Orwell in that: "The true genius is to create a problem and then sell the solution."
 Dirk Verellen, PhD, head of medical physics at UZ Brussel in Belgium.
Dirk Verellen, PhD, head of medical physics at UZ Brussel in Belgium.Verellen presented some examples to reinforce this point. He described the emergence of the multileaf collimator (MLC), which was introduced to replace blocks for shaping treatment fields. Physicists then started to use MLCs for intensity-modulated radiotherapy (IMRT). "A perception was created that you need MLCs to perform IMRT," he said. "Basically, this is not true."
Another example relates to the need to keep the heart out of the radiation beam during radiotherapy of the left breast. This can be achieved using breath-hold methods, and is an important practice in left-breast treatments. But Verellen pointed out that breath-hold can be easily performed, without the need to use "fancy machines."
He emphasized that instead of relying on high-tech systems, it's important simply "to use what you've got." Indeed, sometimes potential treatment improvements are not implemented in the clinic because people think they cannot be achieved without expensive high-tech solutions. He described a student at a recent ESTRO course who claimed that their clinic could not perform image-guided radiotherapy because it only had electronic-portal imaging devices.
The true costs
Verellen pointed out another hazard to consider when implementing new technologies within one of the most complex settings in healthcare: the danger that the focus is too much on innovation and less on safe implementation. "Vendors are selling complex radiotherapy equipment as plug-and-play to facilities with understaffed, undertrained physicists," he explained. "And hospitals are using procedures and workflows that are not adapted to these new systems."
He quoted the celebrated author Terry Pratchett: "New developments cause a rethink. If this bothers you, consider how much damage is being done to the world by people for whom new developments do not cause a rethink."
Meanwhile, the continuous upgrading of software and hardware can lead to an expensive way of working for clinics keen to keep up with the latest advances. There's a real risk that too much focus on expensive, sophisticated technologies may create a double-layer healthcare system.
"The true cost of something is what you give up to acquire it," Verellen said. "If a technology comes at the cost of reducing healthcare for the average cancer patient, it is expensive." And while patients often perceive that the more expensive treatment option must obviously be the best, this is not always the case. "It's not how much it costs, it's the outcome that should be important," Verellen said.
Trials are needed
He emphasized the need for evidence-based medicine and randomized controlled trials, noting that the oft-quoted parachute example (the lack of randomized trials of parachute intervention during free fall Bottom of Form) is not a fair comparison. "Medical devices are more likely to be used when it is clear that their risk/benefit ratio is more favorable than, or at least equal to, current care," he said.
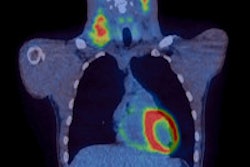
What's needed now, Verellen suggested, is tools that can monitor patients closely and accurately assess the accumulated inter- and intrafraction doses. The focus should be on understanding the biological processes that underlie radiation oncology. And to do this, we need to observe and learn, not from phantoms or cells in petri dishes, but from living, breathing patients.
So is it really the case in radiation therapy that "technology is desperately looking for problems?" Perhaps, but Verellen ended on a positive note, pointing out that in actuality, all stakeholders in this field -- including radiation therapists, vendors, clinicians, and patients -- have a common goal: to cure or ease the pain of the cancer patient.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.