Prize-winning German research has provided compelling new evidence that in many patients with coronary artery disease, late gadolinium enhancement (LGE) cardiac MRI can depict previously unknown myocardial infarction (MI).
"These patients represent almost half of the patients found to have MI. Thus, silent MI has to be regarded as a frequent finding in LGE cardiac MRI," noted Dr. Bernhard Klumpp and colleagues from the department of radiology at Eberhard Karls University Tübingen. "Although these MI are smaller than apparent MI, they are of clinical relevance as the presence of MI is linked to an unfavorable prognosis."
Assessment of myocardial viability is of clinical relevance for risk stratification and subsequent planning of therapeutic strategies and patient surveillance, and in some patients with coronary artery disease (CAD), clinically silent MI can be expected due to either uncharacteristic or lack of symptoms, they stated in an ECR 2015 e-poster that received a cum laude award. First-pass perfusion and LGE cardiac MRI are established techniques to assess myocardial ischemia and MI in patients with CAD.
Klumpp and colleagues studied the frequency of silent MI in patients with clinical symptoms of CAD. A total of 240 patients with symptoms of CAD were assessed retrospectively, comprising 182 men and 58 women. The mean age was 63.5 ± 10.5, and 181 patients had a history of CAD while 76 had a history of MI. Inclusion criteria were either suspected CAD due to new onset of symptoms or known CAD with recurrence of symptoms.
They performed MRI to assess myocardial perfusion and viability in these patients to decide on therapeutic options. All patients were examined on a 1.5-tesla whole-body MR system using a surface-array coil (Magneto Sonata and Avanto, Siemens Healthcare).
The examination protocol included perfusion, functional, and viability imaging. Myocardial perfusion was assessed at stress and rest using 2D saturation-recovery (SR) gradient-echo (GRE) sequences after injection of 0.1 mmol of gadobutrol (Gadovist, Bayer Healthcare) per kg of body weight for each measurement. Myocardial viability was assessed using 2D inversion-recovery (IR) GRE sequences in the four-chamber, two-chamber, and short-axis views 10 minutes after resting perfusion and 20 minutes after stress perfusion. An inversion time localizer was used to determine the optimal inversion time to suppress signal from viable myocardium.
Sequence parameters for LGE cardiac MRI were 2D IR GRE sequence, TR 11 msec, TE 4.4 msec, flip angle 30°, slice thickness 6 mm, baseline matrix 256, and inversion time individually adjusted to 260-340 msec to minimize signal from normal myocardium, Klumpp and colleagues reported. Myocardial function was assessed using cine steady-state free precession (SSFP) sequences.
Regional contrast enhancement of circumscribed shape with base at the endocardial border on LGE images was defined to represent MI. LGE images were assessed in regard to presence, size, and location of MI. The location and supplying coronary artery were assigned according to the American Heart Association's 17-segment model. The size of MI was represented semiquantitatively by the number of affected myocardial segments, and the location of MI was represented by the number of each affected segment.
Patients with MI depicted by LGE cardiac MRI were assigned to two groups: group one consisted of patients with a history of MI, while group two consisted of patients with no history of MI. Both groups were compared regarding size and location of MI, as well as left ventricular function, they explained.
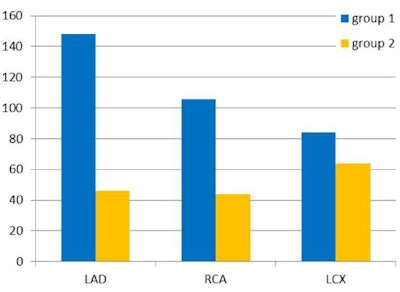 Total number of segments involved in myocardial infarction for each vessel territory compared for patients with apparent (group one) and with silent (group two) myocardial infarction. (LAD = left anterior descending artery, RCA = right coronary artery, LCX = left circumflex artery). Image courtesy of Dr. Bernhard Klumpp.
Total number of segments involved in myocardial infarction for each vessel territory compared for patients with apparent (group one) and with silent (group two) myocardial infarction. (LAD = left anterior descending artery, RCA = right coronary artery, LCX = left circumflex artery). Image courtesy of Dr. Bernhard Klumpp.CAD was confirmed by cardiac MRI and coronary angiography in 210 patients. LGE cardiac MRI depicted MI in 118 of 210 patients with CAD (56%), and CAD was previously known in 110 of the 118 patients with MI in LGE cardiac MRI. In 69 of the 118 patients found to have MI in LGE cardiac MRI, MI was previously known (58%). In group one, 62 men and seven women, the mean left-ventricular ejection fraction was 49 ± 11%, range 18% to 74%, and the MI size was 4.9 ± 3. In 49 of the 118 patients found to have MI in LGE cardiac MRI, MI was previously not known (42%). In group two, 45 men, four women, the mean left-ventricular ejection fraction was 52 ± 11%, with a range of 22% to 72%, and a MI size of 3.2 ± 2.1. There was no significant difference for left ventricular function, and no significant difference for gender distribution.
Patients in group two (silent MI) were significantly older, and MI in group two was significantly smaller. MI in group two occurred significantly more often in the left circumflex artery (LCX) territory and less often in the left anterior descending (LAD) artery territory, with no significant difference in the RCA territory. Silent MI was depicted by LGE cardiac MRI in 27% of patients with previously known CAD and in 23% of all patients found to have CAD, representing 42% of all patients found to have MI by LGE cardiac MRI.
"Our results confirm that chronic MI is a frequent finding in patients with CAD. Yet, 42% of all MI depicted by LGE cardiac MRI throughout the study were not known before," the authors wrote. "These patients with clinical occult MI represent 23% of all patients found to have CAD in the study and 27% of patients with previously known CAD. They have to be regarded as patients at increased risk for major adverse cardiac events."
Furthermore, patients with clinically silent MI were significantly older than patients with a history of MI. This correlates well with the results of other studies, yet in contrast, no significant difference in gender distribution could be found, they added.
Although there was no significant difference between patients with apparent and silent MI regarding left-ventricular function, the size of MI depicted by LGE cardiac MRI was much larger in patients with a history of MI. This could be expected, because larger MI are more probably associated with typical clinical symptoms, the authors pointed out. Moreover, there was a significant difference in location of MI. In patients with previously unknown MI, the lateral and inferior walls supplied by the LCX artery were affected more often, whereas in patients with a history of MI, the anterior wall supplied by the LAD coronary artery were affected more frequently.
Overall, CAD is one of the most common reasons for morbidity and mortality, and often MI is the first clinical manifestation of CAD. In some patients with CAD and no history of MI, the presence of silent MI can be expected due to negligence or lack of symptoms, they summarized. Therefore the assessment of myocardial viability in patients with known or suspected CAD may contribute valuable information for risk stratification.