LONDON - Cardiac MRI should be incorporated into studies of myocardial reperfusion to predict clinical outcomes and provide insight into mechanisms of benefit, attendees of a packed session were told on Monday at the European Society of Cardiology (ESC) annual meeting.
 Perform an MRI scan within the first week of an infarction, Dr. Ingo Eitel advocates.
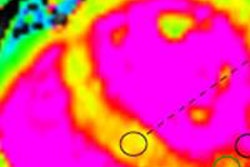
Perform an MRI scan within the first week of an infarction, Dr. Ingo Eitel advocates.Dr. Ingo Eitel, a cardiologist from the Universitäres Herzzentrum Lübeck, Schleswig Holstein, Germany emphasized that cardiac MR has incremental prognostic significance -- in terms of infarct size and microvascular obstruction -- over clinical risk scores and the presence of left ventricular (LV) dysfunction in predicting future cardiovascular events in myocardial infarction.
"Cardiac MR, and especially the presence of late-enhancement imaging, also has a strong prognostic value in almost all cardiomyopathies including myocarditis," Eitel explained. "The current prognostic cardiac MR data warrant future studies to investigate the role of cardiac MR-based decisions in the clinical management of cardiovascular patients."
Beyond measurement of infarct size, assessment of microvascular perfusion by cardiac MRI has prognostic value in the early period after ST-elevation myocardial infarction (STEMI) in patients who are being managed with primary percutaneous coronary intervention. In addition to the management of acute coronary syndromes, cardiac MRI has a prognostic role in nonischemic cardiovascular disease, he told ESC 2015 attendees.
Cardiac MRI's prognostic implications in acute coronary syndromes include visualization of acute myocardial infarction in vivo, predicting adverse clinical outcome (infarct size, myocardial salvage, microvascular obstruction, hemorrhage), risk stratification and incremental value in clinical trials, and as a valid endpoint for reperfusion studies, Eitel continued. In this area, he praised the recent work of the Glasgow group headed by Dr. David Carrick et al, particularly an in-press article in the European Heart Journal.
MRI's role in guiding therapy
For patients who come to the cath lab with signs of acute coronary syndromes but who have clean coronaries, cardiac MRI is of great value for guiding medical therapy because accurate diagnosis can be made in more than 90% of these patients, he added.
Session moderator Dr. Chiara Bucciarelli-Ducci, PhD, from Bristol University Hospital, U.K., asked Eitel about the best procedure for patients with impaired LV function on echocardiography and suspected cardiomyopathies.
"It depends. If the etiology is unknown, everybody gets an MRI to establish the exact diagnosis," Eitel said. "But probably we need more data to have an MRI for all patients."
A Swiss ESC delegate appreciated that Eitel had shown clearly that microvascular obstruction has very important prognostic value, but he asked what time period after infarction should documentation take place and whether the time period of such documentation can also be a prognostic marker.
"We usually perform our infarction MRIs within the first week, but we know from animal studies that infarct size and also microvascular obstruction are dynamic processes, and the longer you wait after an infarction, the greater the chance that an obstruction will have gone and won't be detected by late-enhancement MRI," he said. "In some cases, microvascular obstruction can even persist after several months of the infarction."