Faced with a choice of CT, MRI, and hybrid nuclear imaging for the diagnosis of coronary artery disease, which modality is most suitable for any one patient type and why?
Speaking in favor of hybrid imaging, Dr. Sami Kajander, a radiologist at Turku University Hospital, Finland, succinctly states his reasons for believing a combination of modalities is the best way forward: "Hybrid imaging combines the anatomical detail of CT with the excellent sensitivity of nuclear imaging -- therefore it is more than the sum of its parts."
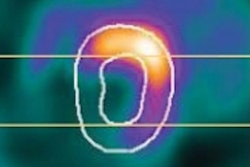
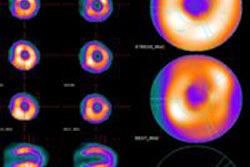
Comparing CT coronary angiography (CTCA) with myocardial perfusion imaging techniques -- single photon emission computed tomography (SPECT) and PET -- for the noninvasive diagnosis of coronary artery disease, he pointed out that both methods have unique strengths and weaknesses. Firstly, CTCA shows epicardial plaques and stenoses, and normal or near normal CTCA effectively rules out significant coronary artery disease with excellent negative predictive value, but is generally unable to provide information about blood flow at the myocardial level. In contrast, nuclear imaging is the gold standard in assessing the myocardial flow and perfusion, but it fails to visualize the epicardial arteries themselves.
Kajander aims to present a convincing argument for the considerable diagnostic benefits of using information gleaned from both imaging modalities. "The main advantage of using hybrid imaging, in the setting of coronary artery disease, is the possibility of obtaining information on both the anatomy and function of the heart in one noninvasive study," he remarked.
In combination, the data from both modalities provide an estimation of the coronary anatomy and the functional consequences of its disease. By way of example, he explained that in coronary artery disease, hybrid imaging overcomes the inability of anatomical imaging to accurately assess the impact of coronary artery stenosis on the function of the myocardium. For instance, it is often not possible to judge on anatomical grounds alone whether the patient will benefit from a coronary bypass operation or coronary stenting -- functional assessment is required to make such a judgment in many cases, he said.
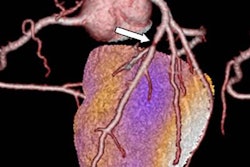
 The availability of 3D volume-rendered techniques has enhanced the clinical value of coronary CT angiography examinations. Images courtesy of Dr. Hatem Alkadhi.
The availability of 3D volume-rendered techniques has enhanced the clinical value of coronary CT angiography examinations. Images courtesy of Dr. Hatem Alkadhi.However, Kajander balanced this with the need for anatomical imaging too, in particular how CTCA can visualize early plaques that may still be nonflow-limiting but already in the remodeling stage of coronary wall disease. "When the disease is evaluated on the grounds of the myocardial function only, even extensive coronary artery wall changes may be left unnoticed if they do not limit coronary flow. This has an impact on secondary prevention, for example medication," he noted, adding that CT gives information about the calcium burden of the coronary tree and as such is valuable in risk stratification and patient management.
Who are the most suitable patients for hybrid imaging? Kajander recommends that patients with intermediate risk for coronary artery disease are the most likely to benefit from hybrid imaging. In this group of patients, CT is noninvasively able to detect both the coronary artery wall changes, including the degree of anatomical stenoses and the composition of the coronary plaques, while the nuclear medicine part (PET or SPECT) is able to determine how the related myocardium is affected.
Specifically, a patient with risk factors for coronary artery disease but only expressing atypical chest pain and unspecific changes in stress test would be a prime candidate for hybrid imaging. To determine whether the patient has coronary artery disease, his or her clinician might order a cardiac PET/CT.
"Let's assume there are extensive coronary calcifications identified in the CT part of the study. It makes it quite difficult to accurately assess the exact degree of possible stenosis, because the calcifications are the greatest single reason for the mediocre positive predictive value of the CT test," he began, explaining a typical scenario.
In addition, functional assessment of how the anatomical findings affect blood flow is required. "Even if we assume that there are only uncalcified plaques, and the anatomical assessment is 100% accurate, it may still not be possible to determine how the anatomical changes affect the myocardial flow: stenoses from about 50 to 70% may reduce the flow -- or they may not," he said.
For this reason, the solution, affording the best outcome for the patient, lies in the hybrid of CT and nuclear modalities, according to Kajander. "When combined with PET or SPECT data, we know both the presence and the severity of the disease, and are able to opt for the best possible treatment."
Arguing the case for single-modality CT imaging, but commenting on how MRI also has an important place in the diagnostic process, is Dr. Hatem Alkadhi, from the Institute of Diagnostic and Interventional Radiology at University Hospital Zurich. He firmly believes that, as with all modalities, selection of the most appropriate patient population for CT is crucial and explained that symptomatic patients presenting with atypical chest pain with a low to intermediate pretest probability of coronary artery diseaseare best suited to undergo imaging with CT.
"CT can then be used as a filter test: If CT is negative, there is no need for further invasive workup. If CT is positive, a stress test such as cardiac MR is recommended for determining the presence/extent or absence of ischemia and infarction," he remarked.
Conversely, a CT examination is inappropriate if patients are asymptomatic, and that is also the case for patients who are symptomatic with typical angina and/or having a high pretest probability of suffering from coronary artery disease based on their cardiovascular risk factor profile, he added.
"CT depicts the coronaries, whereas cardiac MR imaging characterizes the myocardium," Alkadhi explained. "So CT and MR imaging are complementary tools. Each coronary stenosis should be checked for its hemodynamic relevance in terms of myocardial ischemia/infarction prior to revascularization."
In the case of a coronary stenosis detected with CT, stress testing with cardiac MRI should follow. However, when there is no stenosis and no plaque on CT, there is no need for stress cardiac MR, because no ischemia/infarction is expected.
Finally, he turned to findings from recent literature that influenced his opinion of nuclear imaging. "These data convincingly showed cardiac MR imaging to be the superior stress test in terms of diagnostic accuracy. In addition, it is not associated with ionizing radiation."
Dr. Marco Francone, associate professor of radiology at Sapienza University of Rome, presented the case for MRI and pointed out that imaging needed to focus on the identification of ischemic/nonviable myocardium, which may have an impact on a patient's management and outcome.
"There are a number of reasons for this," he stated. "First, myocardial ischemia is not linearly correlated with stenosis degree and represents an important independent prognostic predictor. Second, identification of the culprit lesions producing the ischemia should be mandatory to correctly set up revascularization strategies, and thirdly, the outcome of revascularization improves when demonstrable ischemia is present and effectively treated whereas no clear benefit is usually obtained in presence of stenosis-driven procedures without combined functional-provocative tests."
The importance of cardiac MR in this clinical setting derives from the multiplicity of available techniques within a single study, including rest/stress perfusion, dobutamine stress, and late enhancement, noninvasively and with superior diagnostic performances as compared with direct competitors such as SPECT/PET and echocardiography, according to Francone.
"Using MR imaging means that patients with suspected coronary artery disease can be examined for the presence of ischemia with high accuracy and differentiating between various ischemic entities," he noted.
Regarding which patients were most suitable for MRI as opposed to other modalities, there is a series of clinical indications in which the exam has been recognized as appropriate and may be used as a first-line technique, and Francone outlined some of the clinical indications. "In symptomatic stable coronary artery disease, stress-cardiac MR is highly recommended in intermediate to high-risk patients mostly in the presence of preceding discordant or a not interpretable stress test."
In chronic coronary artery disease, viable and nonviable segments can be discriminated with cardiac MR, and this represents a unique tool to correctly categorize patients who might benefit from coronary revascularization, he concluded.
Originally published in ECR Today on 7 March 2015.
Copyright © 2015 European Society of Radiology