A novel technique developed in the Netherlands promises to determine stenosis severity in coronary CT angiography (CCTA) noninvasively -- and without the complexity of fluid dynamics calculations used in other noninvasive CT examinations, according to an article-in-press posted online on 30 October by the European Journal of Radiology.
Researchers from the University of Groeningen used a technique called corrected contrast opacification (CCO) that measures the difference in Hounsfield contrast attenuation before and after stenosis and correct it for timing using attenuation in the descending aorta. In their study of 60 asymptomatic individuals with CT-detected stenosis in the coronary arteries, CCO showed a strong correlation with hemodynamically significant coronary artery disease (CAD) as determined by a validated noninvasive test, adenosine perfusion MR imaging (APMR).
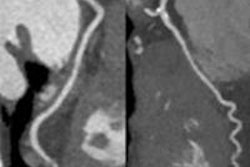
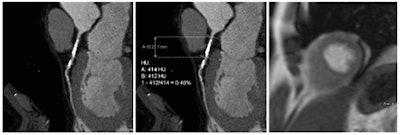 Coronary artery stenosis without hemodynamic significance: CCTA images are at left and center, while MRI (the reference standard for myocardial ischemia) is on the right. Images courtesy of Dr. Rozemarijn Vliegenthart.
Coronary artery stenosis without hemodynamic significance: CCTA images are at left and center, while MRI (the reference standard for myocardial ischemia) is on the right. Images courtesy of Dr. Rozemarijn Vliegenthart."The results show that based on quantitative imaging biomarkers, derived from 'regular' coronary CT angiography, additional information can be gained regarding the hemodynamic significance of a coronary stenosis," Dr. Rozemarijn Vliegenthart wrote in an email to AuntMinnieEurope.com. "This is important because a large part of coronary narrowings with > 50% lumen diameter stenosis do not cause myocardial ischemia."
When corrected for length, composition, and location of stenosis, the drop in CCO remained significantly different for hemodynamic stenosis versus those without hemodynamic significance, wrote Vliegenthart, lead author Dr. Martijn den Dekker, and colleagues.
Coronary CT angiography shows high accuracy for the detection of coronary artery disease, but it shows poor correlation with myocardial ischemia.
"A large part of coronary narrowings with > 50% lumen diameter stenosis do not cause myocardial ischemia," Vliegenthart explained in her email. "We are investigating ways in which a single noninvasive test can provide comprehensive information about coronary artery disease, so not only anatomical but also functional information."
FFR versus FFR-CT versus COO
A technique called fractional flow reserve (FFR) is used in catheterization labs to measure the effects of coronary stenosis on myocardial perfusion. But because FFR is invasive it carries costs and risks, and as a result is used (and remains ethical) only in symptomatic patients.
Fractional flow reserve CT (FFR-CT) measures flow noninvasively by analyzing CT images using principles of fluid dynamics, and a couple of systems are currently being validated, one that involves sending images to an offsite lab, and a newly introduced technique that performs the FFR computations onsite, saving time and money. A third noninvasive technique based on CT attenuation like FFR-CT, but not involving fluid dynamics, was examined for this study.
"One of the methods currently under investigation is CCO measurement," Vliegenthart told AuntMinnieEurope.com. "This measurement is based on a different principle than FFR-CT, as no computational fluid dynamics is used, but measurement of the gradient of CT density along the coronary artery. This is a semiautomated measurement with little reader interaction that can be performed on-site using dedicated software, in contrast to FFR-CT. We found excellent inter-reader agreement in a sub study (part of the manuscript). However, we did not compare these techniques directly, so we cannot state how well they compare in terms of outcomes."
This study compared its COO results with APMR, which has high sensitivity of 91% and specificity of 94% as compared with invasive FFR. The researchers examined 60 asymptomatic cardiac patients with extracardiac arterial disease (mean age 64.4 ± 7.7 years; 78% male) who underwent both CCTA and APMR. The study measured luminal CT attenuation values, or Hounsfield Units, in the coronary arteries from proximal to distal, with additional measurements across sites showing greater than 50% stenosis at CCTA.
Following injection of iodinated contrast (Iomeron 400, Bracco Diagnostics), the images were acquired on a dual-source CT scanner (Somatom Definition, Siemens Healthcare) using ECG gating at 64 x 2 x 0.6 mm by z-flying spot with 0.4-mm increments, and 120 kV, with tube voltage and current based on weight.
An experienced attending radiologist evaluated the coronary artery images on CT; reconstructed as axial images and curved planar reformats (Syngo software, Siemens Healthcare).
CT was performed prior to APMR on a 1.5-tesla scanner (Siemens Healthcare). CCO was calculated by dividing coronary CT attenuation by descending aorta CT attenuation. In the study, a reversible perfusion defect on APMR was considered to be myocardial ischemia, the authors wrote.
At APMR, the most likely culprit artery for the perfusion defect was assessed, the authors wrote. In patients with perfusion defects, the group labeled all anatomically significant stenosis in the culprit artery as hemodynamically significant.
Excellent correlation to APMR
The study team found 169 coronary stenoses in total, including 67 in the left anterior descending artery (LAD), 32 in the circumflex artery (LCX), and 60 in the right coronary artery (RCA). Fifty-nine stenosis cases were caused by partially calcified plaque, 109 by calcified plaque, and one by soft plaque.
Among the anatomical stenoses, 68 narrowed the lumen diameter by 50% or more, and 14 lesions by more than 70%. No stenosis less than 50% showed hemodynamic significance.
The drop in CCO across vessels with hemodynamically significant stenoses was larger than that of vessels without associated ischemia, the group reported. The CCO decrease across stenoses with hemodynamic significance was 0.144 ± 0.112 versus 0.047 ± 0.104 across stenoses without hemodynamic significance (P = 0.003). Meanwhile, the CCO decrease in lesions with and without anatomical stenosis was similar (0.054 ± 0.116 versus 0.052 ± 0.101; P = 0.89).
Using a CCO decrease of 0.20 as a preliminary cut-off, the hemodynamic significance of a lesion would be excluded in 82.9% of anatomical stenosis, den Dekker et al reported.
"In this study, CCO, derived from common CCTA data, showed a strong association with hemodynamically significant CAD, as determined by APMR," the authors wrote. "For mere anatomical stenoses, no such relationship was present. These results suggest that additional information from standard CCTA data may assist in differentiation between a coronary stenosis with and without hemodynamic significance."
Many coronary stenoses do not cause a relevant reduction in coronary flow, and it is difficult to predict which anatomical stenosis causes ischemia, the authors wrote. As a result it is almost always necessary to assess the hemodynamic significance of a CT-detected lesion.
In this study, the prevalence of stress-induced ischemia by APMR was considerable at 12% of patients, a very relevant finding considering that symptomatic patients with a positive ischemia test have a 3.6- to 3.9-fold increased risk for coronary events over the next five years.
"Compared to FFR, APMR has an excellent diagnostic accuracy," they wrote. "However, the (patho)physiological processes underlying CCO and APMR are different." FFR and CCO both examine coronary flow, while APMR and SPECT assess myocardial perfusion.
"We found a good correlation between CCO and APMR, indicating the possibility for a single examination to identify hemodynamic significance of coronary stenoses on top of anatomical severity," they noted.
Compared with previous reports on CCO, the method in this study was slightly altered, and based on semiautomated Hounsfield Unit measurements using curved multiplanar reconstructions. The method produced high reproducibility and excellent inter-reader agreement. An advantage of this approach is that CCO assessment requires less skill and may be performed faster and perhaps more easily in clinical practice.
"We have studied a group of cardiac asymptomatic individuals at high risk of CAD, who underwent cardiac imaging as part of a research study," Vliegenthart told AuntMinnieEurope. "As we obtained adenosine perfusion MRI additional to coronary CTA in all participants in this study, we know which coronary artery stenoses resulted in myocardial ischemia," a number that turned out to be a minority of stenosis as published previously in the European Journal of Vascular and Endovascular Surgery, she stated.
"We are currently considering to evaluate CCO as well as other quantitative imaging biomarkers on coronary CTA in symptomatic patients, to validate and confirm the findings," Vliegenthart wrote. "At this moment, CT is the most promising technique to serve as comprehensive noninvasive test for CAD."