Treating asymptomatic extracoronary artery disease provides no extra benefit to high-risk patients compared with a less aggressive approach that treats only symptomatic disease, according to a report presented on Monday at the European Society of Cardiology (ESC) congress in Rome.
French researchers presenting results of the AMERICA trial (Active Detection and Management of the Extension of Atherothrombosis in High-Risk Coronary Patients in Comparison with Standard of Care for Coronary Atherosclerosis) found no significant differences in outcomes between the intensive and standard approaches to extracardiac disease.
Differences between the aggressive and standard approach for two-year all-cause mortality, rehospitalization for an ischemic event, or organ failure were statistically insignificant, reported lead investigator Dr. Jean-Philippe Collet, PhD, from the Institut de Cardiologie at L'hôpital de la Pitié Salpêtrière in Paris.
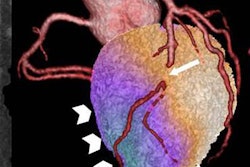
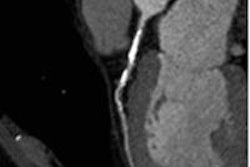
The prevalence and the risks associated with asymptomatic extracoronary lesions in patients at high risk of coronary artery disease are unknown, and the same goes for the benefit of systematic identification and treatment, Collet said in a statement accompanying the study's release.
Aiming to determine the benefit of treating asymptomatic extracoronary lesions, the researchers enrolled 521 patients at high risk of coronary artery disease owing to recently diagnosed three-vessel disease or acute coronary syndrome in patients 75 years and older.
They randomized patients to one of two strategies: a proactive prevention scheme including revascularization of asymptomatic multisite artery disease when appropriate, lifestyle changes, and an aggressive pharmacological approach (n = 263); or to a conventional strategy based on treatment of coronary disease and only symptomatic extracoronary lesions (n = 258).
No impact for extracardiac diseaseWith regard to the primary endpoint, the investigators found no difference between the groups for death, any ischemic event leading to rehospitalization, or evidence of organ failure during the two-year follow-up period.
With regard to the secondary endpoint, they saw no differences between the groups in the rate of all-cause death, myocardial infarction, stroke, or revascularizations, which occurred in 12.9% of the group treated intensively versus 13.6% of those treated conventionally (hazard ratio: 0.94; 95% confidence interval, 0.58 to 1.50).
Even major bleeding was statistically the same between the aggressive treatment (4.6%) and conventional treatment groups (5.0%).
While the aggressive strategy did identify asymptomatic multisymptom artery disease in 23% of patients and led to aggressive secondary prevention in 45.3% of patients, it has produced very few additional revascularization procedures (3.6%) and, ultimately, conferred no clinical benefit over conventional management, Collet and colleagues concluded.
"Possible explanations for the failure of the proactive strategy were that revascularization of [multisymptom artery disease] lesions was rare and that pharmacological treatment was close to optimal in both groups," Collet said in his statement. "This study has important practical implications for daily life."