Pinpointing flow problems in the peripheral arteries is a task that is typically handed over to dynamic MR angiography. But often, bone-subtracted 4D CT angiography (CTA) can do a better job, according to German researchers.
With radiation doses for dynamic CT falling dramatically in recent years, the modality has recently become a viable option for time-resolved dynamic imaging of the peripheral vessels. At University Medical Centre Mannheim in Germany, 4D dynamic CT is delivering markedly cleaner images in patients who can't hold their legs still for a lengthy MRA examination, according to a recent presentation at the International Symposium on Multidetector-Row CT (MDCT 2014) by Dr. Thomas Henzler.
 Dr. Thomas Henzler
Dr. Thomas Henzler"We think that 4D CT imaging can sometimes replace dynamic MRA," said Henzler, who heads CT and cardiothoracic imaging at the university's Institute of Clinical Radiology and Nuclear Medicine. "The main competitor in our department was dynamic MR angiography, and the main motivation for us to integrate 4D CT was that we were really happy with the results for most patients, but [for others] there were problems with motion artifacts and we believe it's much easier for patients to remain still for 45 seconds when compared with 20 minutes for MRA."
Some 60 km down the road, radiologists from the University of Munich had actually looked at 4D CTA a little earlier and found that it significantly improved specificity compared with standard CTA, Henzler said. From those findings, the group at Mannheim has begun using the technique to better understand the location and dynamics of peripheral artery stenosis.
"Especially in patients with heavy calcifications sometimes we find it hard to differentiate between contrast material and calcifications," he said. Comparing both acquisitions together over time makes it clear which phenomenon is occurring because the attenuation of the calcium remains constant as contrast comes and goes in different phases.
The Mannheim way
The dual-step peripheral runoff protocol that researchers are working on at the University of Mannheim starts with a standard CTA runoff protocol, he said. The team uses 45 cc of contrast material for the standard CTA, then uses the bolus-tracking information to determine the optimal scan delay before starting the runoff study.
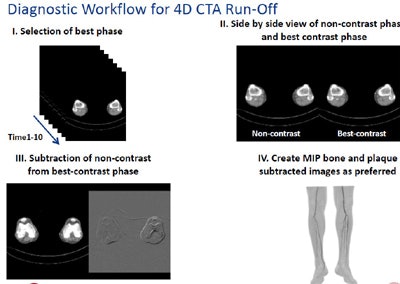
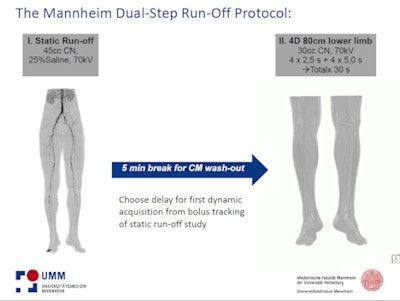 The Mannheim protocol. All images courtesy of Dr. Thomas Henzler.
The Mannheim protocol. All images courtesy of Dr. Thomas Henzler."We need the patient to wait five minutes on the table for the contrast to wash out and then we start our dynamic runoff study," Henzler said. Why is this crucial? Because, for example, in a patient with a high-grade stenosis of the common iliac artery the principal question is what's happening in the lower limb, which makes the temporal information very valuable, he said.
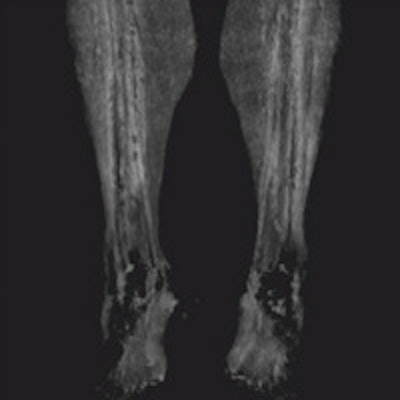
When the vessels in the lower leg are heavily calcified it's hard to tell what's going on with dynamic MRA. But acquire the images with dynamic CT, then subtract the bone, and the calcium and status of the blood flow is revealed, he said.
When the noncontrast series of images are subtracted from the bone-subtracted contrast-enhanced dynamic series, "you can finally see there is still sufficient runoff in the area of the heavy calcified plaque that is also subtracted when you subtract the complete noncontrast scan from the dynamic series," he said. And happily, the patient gets to skip the intervention.
 Patient with lower-limb calcifications. Dynamic bone-subtracted dynamic CTA (below) separates the contrast from the calcifications.
Patient with lower-limb calcifications. Dynamic bone-subtracted dynamic CTA (below) separates the contrast from the calcifications.
What you don't want to do is send all 13,000 static and dynamic images from a single patient scan to your PACS network, Henzler said. The data load can be trimmed substantially by sending only the arterial reconstruction or maximum intensity projection (MIP) datasets to the PACS. It's enough images to give patients and referring doctors a sense of what's going on in the region, and help them integrate the 4D information, he noted.
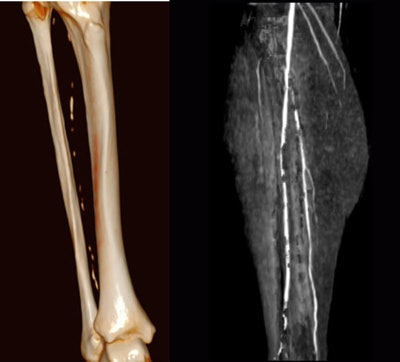
Evaluating the patency of peripheral stents is another scenario where dynamic CT can be a game-changer, according to Henzler. For example, in a patient with suspected occlusion of a popliteal stent, the standard image series shows antegrade blood flow at the beginning and throughout the stent -- and antegrade flow is a key indicator of high-grade stenosis.
Wider coverage
In another comparison with dynamic MRA, CT's main advantage was its wider anatomic coverage that encompassed the entire stent region -- 80 cm of z-axis coverage with dynamic 4D CTA versus 40 cm for 4D MRI. The second advantage was that the patient couldn't hold his legs still for a long MRI study, and CT eliminated the motion artifacts, enabling diagnosis.
Again, PACS should receive only selected images. "Workflow is important when you have large amount of patients," he said, and sending only the standard acquisition and the best dynamic contrast CT phase to the PACS saves space and reading time.
 Sending only MIPs to the PACS saves storage space and reading time.
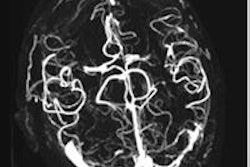
Sending only MIPs to the PACS saves storage space and reading time.Dialysis shunt imaging is another application where 4D CT can help reveal blood-flow dynamics, unearthing substantially more information about the stenosis, pinpointing the location precisely. Such temporal information can reveal how conditions such as shunt steal are occurring.
"In summary, I think it is an interesting way to diagnose, using 4D imaging for certain applications," Henzler said. Using low kV settings, "the radiation dose is now becoming acceptable, and it might be more robust than MRI for really ill patients."