Coronary CT angiography (CCTA) significantly outperformed coronary calcium scoring for predicting cardiac events in asymptomatic individuals, concludes an Austrian study presented at the European Society of Cardiology meeting (ESC 2014), held last month in Barcelona, Spain.
The study included more than 700 asymptomatic individuals at high risk of coronary disease who underwent CCTA and coronary artery calcium scoring (CCS), as well as invasive coronary angiography. After almost three years' mean follow-up, CCTA results were found to be highly predictive of major adverse cardiac events (MACE), while having five or more involved segments increased the risk sixfold.
 Dr. Fabian Plank from Innsbruck Medical University.
Dr. Fabian Plank from Innsbruck Medical University.At the same time, half of the individuals had no measurable coronary calcium, but CCTA found noncalcified plaques in nearly one-third, the study team reported.
"Based on our results, we observed a clear superiority of CCTA over CCS in terms of accuracy for predicting MACE and revascularization, similar to recent data released from the CONFIRM registry," Dr. Fabian Plank from Innsbruck Medical University wrote in an email to AuntMinnieEurope.com.
CCTA adds valuable information over the calcium score in detecting noncalcified plaques, and quantifying plaque burden while also allowing for structural and dynamic volume assessment, he noted. "Therefore CCTA proves to be more accurate to stratify a patients' cardiac risk of adverse outcome, as compared with calcium scoring alone."
High risk of CAD
In the study, 711 consecutive asymptomatic patients (mean age 61.8 years, 40% women) with a high lifetime risk of coronary artery disease were examined with CCS as well as CTA. Stenosis at CCTA was rated mild (< 50%), intermediate (50% to 70%), or high-grade (> 70%).
"We evaluated CCTAs to find predictive factors for adverse cardiac outcome and compared them with CCS, which is currently the test of choice according to the ACF/AHA guidelines," Plank said. ECG stress testing is one of the most commonly performed tests, but due to the low sensitivity and specificity of 60% to 70%, both false positives and negatives have to be considered. CCTA is in a different class entirely.
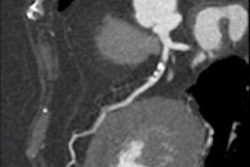
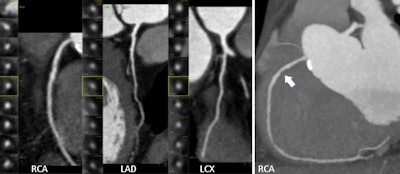 CCTA finds significant coronary artery disease in symptomatic 64-year-old man. Patient has hyperlipidemia and a family history of coronary disease; is an ex-smoker. Patient also underwent a nonspecific pathologic stress test. All images courtesy of Dr. Fabian Plank.
CCTA finds significant coronary artery disease in symptomatic 64-year-old man. Patient has hyperlipidemia and a family history of coronary disease; is an ex-smoker. Patient also underwent a nonspecific pathologic stress test. All images courtesy of Dr. Fabian Plank. Two years (680 days) later, patient had ACS (STEMI), right coronary artery (RCA) stenosis of 100%, CKmax 1,416 ng/dL, TNTmax 3,315 ng/L.
Two years (680 days) later, patient had ACS (STEMI), right coronary artery (RCA) stenosis of 100%, CKmax 1,416 ng/dL, TNTmax 3,315 ng/L.CCTA is a highly accurate modality for these patients, he stated. SPECT and MRI are performed less often owing to limited availability and high cost, especially locally in a largely rural atmosphere where few scanners are available.
How many, how severe, how calcified?
The protocol required adding up the number of involved coronary segments (segment involvement score) for each patient, and measuring the CCS at CCTA. CCTA-detected plaque was characterized as calcified or noncalcified, and graded stenosis in each segment in plaque was present at 50% or less luminal narrowing as mild, 50% to 70% as intermediate, and 70% or greater as high-grade stenosis.
Major adverse events such as ST-elevated myocardial infarction (STEMI), non-ST-elevated myocardial infarction (NSTEMI), and cardiac death served as the primary study endpoints, while coronary revascularization procedures like percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) served as secondary endpoints.
Among the 711 high-risk patients, just more than one-fourth (28.3%) were negative for coronary artery disease while 71.7% were positive at CCTA, the group reported.
As for disease severity in these asymptomatic individuals, CT showed that 15.6% had plaques without stenosis, 23.9% had mild plaque, 10.7% had intermediate plaque, and 21.5% had high-grade stenosis of 70% narrowing or greater, the authors reported. A zero calcium score didn't mean the arteries were clear.
In fact, plaque was found in 43% of patients, and noncalcified plaques were seen in 100 (32.7%) of all patients with zero calcium scores.
Over a mean follow-up period of 2.65 years with a maximum of eight years, the rate of MACE was 0% in CAD-negative patients and higher (1.2%) in patients whom CCTA showed to have coronary artery plaque.
More segments, more events
Patients with five or more involved segments had a hazard ratio of 6.49 (95% CI: 1.63-25.76, p < 0.013) for major adverse cardiac events, while patients with a noncalcified segment involvement score of 1 or greater had a hazard ratio of 2.36 (95% CI: 1.20-4.63, p < 0.01) as a secondary endpoint. The coronary revascularization rate was 5.5%.
Thus, an increasing number of involved segments definitely upped the risk of events. Was it a steady increase or did it spike with increasing involvement scores?
"The total plaque burden certainly increases the risk for adverse outcome," Plank said. "We used a stepwise testing approach to find that the risk increased quite steadily to a threshold of segments and then plateaued at similar hazard. Interestingly, noncalcified plaques only seemed to have a higher predictive value than the plaque burden in total. This may be explained by the fact that an (unknown) percentage of those noncalcified plaque [patients] have high-risk features, for which we didn't look in detail yet."
Even so, the knowledge is important because a high number of myocardial infarction happens in patients without prior symptoms, Plank stated. Fortunately, doctors are finally starting to refer more high-risk patients to CT. Should all high-risk individuals, even completely asymptomatic, be referred to CCTA?
"The time is right!" Plank wrote. CCTA adds valuable information over a simple calcium score in detecting noncalcified plaques, measuring plaque burden, and providing structural and dynamic volume assessment.
CCTA has been shown to be more accurate to stratify a patients' cardiac risk of adverse outcome, as compared with calcium scoring alone. And doctors are starting to catch on, he said.
"We do see a shift towards increasing referrals of asymptomatic patients with high-risk profile to CCTA -- from many cardiologists," he wrote. The feedback from interventional cardiologists along with this trend is very positive though. Catheterization lab cardiologists recently reported relatively increasing numbers in positive procedures and reducing number of diagnostic caths -- which is a very positive trend for both patients and physicians. Not everyone is on board with CT referrals for everyone at high risk, however.
"How to screen asymptomatic patients is still an open and hot debate," Plank stated.
The group plans to continue its follow-up of the study patients, and will probably add fractional flow reserve-CT, which has shown a lot of promise in assessing the severity of stenosis, to future exams, he said.