Digital radiography (DR) is a good tool for detecting cases of methamphetamine body packers, according to a new study in the British Journal of Radiology. But the unique nature of such radiography studies may call for additional training when radiologists are called to interpret images of suspected drug carriers.
That's according to researchers from Malaysia, who reported on the unique challenges of imaging drug carriers (BJR, 28 January 2014).
In East and Southeast Asia, methamphetamine and its derivatives, known as "syabu" or "ice," are more prevalent than cocaine or heroin. Recently, an increasing number of drug carriers, or "mules," have been intercepted by law enforcement at the borders of Malaysia, with some ingesting drug packets or inserting them into body cavities.
The generally accepted radiological exam is a plain abdominal radiograph in the supine position. However, the detection rate for drug-filled packets is highly variable in the literature, and sensitivities ranging from 58.3% to 90% have been reported. Thus, plain abdominal radiography is considered a flawed screening method for identifying drug mules.
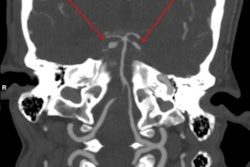
 This patient swallowed 64 packs and displays the double condom sign (packs imaged longitudinally) and halo sign (packs imaged transverse). The forensic imaging inexperienced group counted 31 to 50 packs, whereas the forensic imaging experienced group both counted 60 packs -- again under-reporting the entire internal payload. All images courtesy of Dr. Patricia Flach.
This patient swallowed 64 packs and displays the double condom sign (packs imaged longitudinally) and halo sign (packs imaged transverse). The forensic imaging inexperienced group counted 31 to 50 packs, whereas the forensic imaging experienced group both counted 60 packs -- again under-reporting the entire internal payload. All images courtesy of Dr. Patricia Flach.There is little research on the accuracy of plain abdominal radiography in methamphetamine drug carriers, although there has been a significant increase of meth in Asia. Dr. Saiful Nizam and Abdul Rashid, from the department of radiology at University Putra Malaysia in Selangor, and colleagues retrospectively evaluated the sensitivity, specificity, and accuracy of abdominal DR for identifying the internal payloads of methamphetamine in drug mules.
Their study included 35 individuals suspected of carrying internal methamphetamine drug containers. A total of 59 supine digital radiographs (Polydoros LX 80, Siemens Healthcare) were collected. The gold standard was the presence of secured drug packs in feces.
Sixteen true-positive drug mules were identified. Two groups read the radiographic images. Group 1 consisted of readers experienced in forensic imaging, and group 2 consisted of inexperienced readers.
| Accuracy of DR for identifying drug mules | |||||
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | |
| Group 1 | 100% | 76.3% | 78.5% | 100% | 87.2% |
| Group 2 | 93.7% | 86% | 86.5% | 94.1% | 89.5% |
How to identify drugs radiographically
In all confirmed drug carriers, the "double-condom" and "halo" signs (100%) were detected by each radiologist, Rashid and colleagues found.
"These radiological signs occur due to inevitable air inclusion during manufacturing of drug packets, which creates the specific double-condom sign if the pack is projected longitudinally or the halo sign if it is imaged transversely," they wrote. "However, the 'rosette' sign (due to trapped air at the twisted end of a pack) is not easy detectable on plain radiograph and was only reported in a single (6.25%) case by one radiologist in the experienced group."
Other signs include the "tic-tac" and "parallelism" signs, which are created by the parallel arrangement of longitudinal packs within the large bowel (seen in three cases). Suspicious gas formation in the rectum was reported in two cases by one radiologist in the inexperienced group, but these cases were confirmed to be negative.
"Suspicious geometrical-shaped gas formation may be an indicator for internal drug containers but cannot be used as a reliable sign," the researchers added.
 A case with a huge internal payload within the small and large bowel displaying the double condom sign and alignment of the packs representing the tic-tac sign. Radiological interpretation tends to under-report the total amount. In this case, the radiologists counted 45 to 66 concealed packs. The actual internal payload was 84 packs, collected from the feces as evidence.
A case with a huge internal payload within the small and large bowel displaying the double condom sign and alignment of the packs representing the tic-tac sign. Radiological interpretation tends to under-report the total amount. In this case, the radiologists counted 45 to 66 concealed packs. The actual internal payload was 84 packs, collected from the feces as evidence.In terms of density, two (12.5%) of the 16 positively identified drug carriers were graded with an opacification of 3, meaning the packs were more opaque than the surrounding soft tissue. The remaining 14 (87.5%) cases were classified as 1 or 2 in equal numbers.
In terms of shape, nearly all the drug mules (93.75%) ingested typically shaped longitudinal or tubular body packs wrapped in plastic or condoms. The longitudinal or tubular shape was observed in each case (100%) on imaging, whereas the round shape was observed in one (6.25%) case by all radiologists.
In terms of size, the average length of the longitudinal packs was 4.93 cm (range, 2.5-6.8 cm; median, 5.0 cm) and the width was 2.12 cm (range, 1.4-3.1 cm; median, 2.1 cm). The round drug packs measured 2.0 cm to 5.6 cm in diameter, with an average diameter of 3.18 cm (median, 2.5 cm). The shapes and size measurements on DR were correct according to the measured packs in the feces.
Limitations of DR
Assessing the total number of internal drug containers is where DR falls short due to the overlapping of the packs within the gastrointestinal tract and concomitant summation, especially in cases with huge payloads, the researchers found. The average payload was 39 packs on DR (range, 0-75; median, 41).
The assessment in group 1 of the internal payload was better, with 79.0% accuracy compared with 59.0% in group 2.
The mean number of packs secured from the feces was 65 (range, 12-111; median, 70). However, DR had a noted tendency to underreport in 13 (81.3%) of the 16 cases compared with the number of secured packs; overreporting was only observed in three (18.7%) cases.
The researchers acknowledge their study yielded a higher diagnostic accuracy than has been reported in most of the recent literature, which can be explained by the small sample size and almost homogeneous study population (i.e., primarily body packers with huge internal payloads consisting of typically longitudinal shapes).
Also, 100% of the patients had drug containers within the large bowel and rectosigmoid region; containers in these areas are easier to assess on DR than those in the small intestine or stomach, because there is less summation and a greater accumulation of packs within the lumen, the researchers wrote.
Another limitation of the study was the potential for manipulation of the internal payload by the perpetrator, because the mules were not continuously monitored and no dedicated holding cell or drug toilet was available.
"Therefore, false positives on imaging may not have been truly false positives, and the suspect may have managed to discharge the drug container and dispose of it (e.g., dissolved in supplied drink or food or hidden in small gaps in the wall)," the researchers noted.
Conclusion
All investigators underestimated the internal payload in 81.3% of cases, although readers in group 1 were more accurate.
"This finding substantiates the need for image reading training in drug carrier cases, awareness of the typical radiological findings in such cases, and may favor cross-sectional imaging rather than conventional x-ray in drug carriers," the researchers wrote.
Conventional imaging allowed for no weight estimation, but CT imaging would allow for segmentation of the internal drug containers and may also allow for weight estimation, Rashid and colleagues noted.
"Regarding medicolegal issues, especially in countries with draconian drug laws, based on the diagnostic insecurity on plain films in this underlying study and on recent research, low-dose CT may offer a more reliable alternative to DR to increase diagnostic security," the researchers concluded. "Training radiologists in reading drug carrier images should be obligatory to increase the specificity of detection on imaging and to overcome literally walking on 'thin ice.' "