MRI is the imaging modality of choice for suspected bone or joint complications arising from injected drug use, while CT and ultrasound play a key role in the assessment of soft tissue and vascular complications, Irish researchers have reported.
The clinical presentation of patients may vary and be nonspecific, making timely recognition of imaging manifestations important, noted Dr. Francis Delaney, radiology specialist registrar at Mater Misericordiae University Hospital in Dublin, and colleagues in an article posted on 26 August by Insights into Imaging.
"We work in an inner-city hospital, and these patients make up a decent percentage of our emergency work directly or indirectly in terms of trauma," he told AuntMinnieEurope.com. "Ultrasound and CT would be used quite commonly, and we have a CT scanner in the emergency department as well as in the department. MRI is used more sparingly."
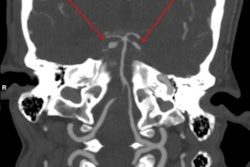
 MRI is the imaging investigation of choice in osteomyelitis and other bone and joint infections. Sagittal T1-weighted (left) and short-tau inversion recovery (STIR) (right) images demonstrate osteomyelitis of the posterior aspect of the calcaneus. Cortical erosion and loss of the normal T1 hypointense rim at the bone edge is seen on the T1 image. There is high STIR signal and corresponding low T1 signal of the posterior calcaneus representing bone edema (red arrow) and overlying soft tissue inflammation is also seen. Images courtesy of Insights into Imaging.
MRI is the imaging investigation of choice in osteomyelitis and other bone and joint infections. Sagittal T1-weighted (left) and short-tau inversion recovery (STIR) (right) images demonstrate osteomyelitis of the posterior aspect of the calcaneus. Cortical erosion and loss of the normal T1 hypointense rim at the bone edge is seen on the T1 image. There is high STIR signal and corresponding low T1 signal of the posterior calcaneus representing bone edema (red arrow) and overlying soft tissue inflammation is also seen. Images courtesy of Insights into Imaging.Illicit drug use appears to be increasing, and it is a significant healthcare problem associated with myriad multisystem complications, the authors explained. The estimated number of people who have used drugs globally rose from 4.8% to 5.5% between 2009 and 2017, and almost 1 in 10 adults ages 16-59 in the U.K. report illicit drug use in the last year.
"Musculoskeletal and vascular complications are commonly seen," the authors pointed out. "The history of illicit drug use is often not forthcoming. A focused multimodal imaging approach is typically required, depending on the nature of suspected complications."
Usefulness of MRI
The MRI sequences employed in suspected soft tissue infection typically include T2, a fluid-sensitive sequence such as short-tau inversion recovery (STIR), and unenhanced and postcontrast T1. Diffusion-weighted imaging (DWI) may be added in certain cases, such as to assess for abscess formation, and fat-saturated T2 or enhanced T1 sequences can be used to improve the delineation of inflammation, Delaney and colleagues continued.
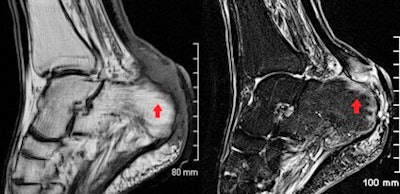
 Images from an intravenous drug user who presented with wrist pain and swelling. Lateral radiograph (A) shows a linear lucency with cortical disruption at the dorsal aspect of the distal radius (white arrow). In the absence of a history of trauma, this was consistent with inadvertent direct injection to the bone. Associated early osteomyelitis is seen on MRI with sagittal STIR (B) showing a linear region of high signal with corresponding hypointense signal on the coronal T1 image (C).
Images from an intravenous drug user who presented with wrist pain and swelling. Lateral radiograph (A) shows a linear lucency with cortical disruption at the dorsal aspect of the distal radius (white arrow). In the absence of a history of trauma, this was consistent with inadvertent direct injection to the bone. Associated early osteomyelitis is seen on MRI with sagittal STIR (B) showing a linear region of high signal with corresponding hypointense signal on the coronal T1 image (C).A gradient echo sequence may be added in more severe cases with suspected hemorrhage or necrotizing fasciitis. In cellulitis, high T2 and STIR signal intensity with corresponding T1 signal intensity of the subcutaneous tissues with overlying skin thickening is seen, and there is enhancement following gadolinium administration.
"MRI provides the most accurate evaluation of the extent of deeper infections and of surrounding soft tissue anatomy and can also assess for associated abnormality of adjacent bones or joints," they wrote. "On MRI, soft tissue abscesses demonstrate internal high T2 and STIR signal with corresponding low T1 signal, peripherally enhancement following intravenous gadolinium administration and restrict diffusion on DWI."
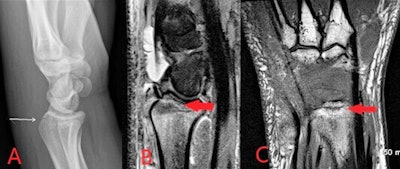
 Axial proton density weighted (A) and sagittal STIR (B) MR images from the same patient as previous figure, demonstrating large volume fluid within the extensor compartment tendon sheaths at the wrist in keeping with septic tenosynovitis associated with injected drug use.
Axial proton density weighted (A) and sagittal STIR (B) MR images from the same patient as previous figure, demonstrating large volume fluid within the extensor compartment tendon sheaths at the wrist in keeping with septic tenosynovitis associated with injected drug use.MRI protocols for suspected bone and joint complications of injected drug use should include a fluid-sensitive sequence such as STIR, in addition to T2 or proton density and T1-weighted sequences in at least two planes. Bone marrow edema is the earliest imaging finding identifiable in acute osteomyelitis and appears on MRI as high T2 and STIR signal intensity of the bone with corresponding low T1 signal. Enhancement following contrast administration is also seen.
High T2/STIR signal without low T1 signal is less specific and may represent reactive osteitis rather than osteomyelitis. Cortical bone destruction can be identified as loss of the normal peripheral T1 hypointense cortical rim. Assessment of the extent of the infection in adjacent soft tissues, differentiation of bone from soft tissue infection and surgical planning can also be reliably achieved on MRI, according to the authors.
MRI is extremely sensitive in the detection of septic arthritis, but findings are nonspecific and can overlap with inflammatory arthritis. MRI protocols typically involve T1, T2, fluid-sensitive (such as STIR) and gadolinium-enhanced sequences.
"MRI may be performed where there is diagnostic uncertainty or for the evaluation of surrounding soft tissues and bones," Delaney et al wrote. "MRI will show a joint effusion with synovial thickening and enhancement, indicative of active synovitis. In chronic infections, destruction of the joint surfaces and periarticular structures occurs with resultant deformity and reactive sclerosis."
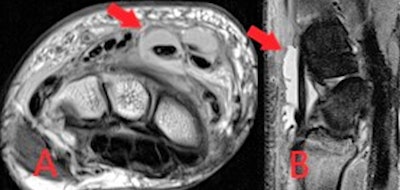
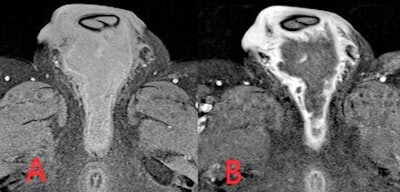 Axial fat-saturated T1-weighted MR images precontrast (A) and postintravenous contrast (B) administration. An intermediate/low intensity defined collection is demonstrated within the perineum. Avid peripheral mural rim-enhancement is seen with nonenhancing internal abscess contents.
Axial fat-saturated T1-weighted MR images precontrast (A) and postintravenous contrast (B) administration. An intermediate/low intensity defined collection is demonstrated within the perineum. Avid peripheral mural rim-enhancement is seen with nonenhancing internal abscess contents.Looking to the future, the Dublin group plans to look at patients with former intravenous drug users who present months or years later with delayed complications or medical disorders related to their previous drug use, Delaney said.