CHICAGO - High tumor stiffness at shear-wave elastography appears to predict lymph node metastasis in women with invasive breast cancer, and automated breast ultrasound (ABUS) turned in a similar diagnostic performance to handheld ultrasound, according to two studies presented on Sunday at the RSNA meeting.
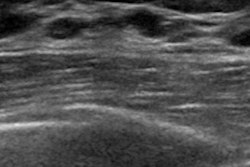
Shear-wave elastography
Higher lesion stiffness values at shear-wave elastography have been shown to be linked with poorer prognoses, said Dr. Andrew Evans, of the University of Dundee in Scotland. Evans and colleagues conducted a study of 396 patients with invasive breast cancer who were treated by primary surgery and had shear-wave elastography at the time of diagnosis. Of this group, 217 were symptomatic, while 179 had screen-detected cancer.
The researchers used SuperSonic Imagine's Aixplorer ultrasound system to find mean stiffness values, taking measurements from a region of interest identified as the stiffest part of the abnormality. The team also assessed associations between lymph node involvement and mean lesion stiffness in kilopascals, invasive cancer size, histological grade, tumor type, estrogen (ER) and human epidermal growth factor (HER2) receptor status, and vascular invasion.
Median tumor size was 19 mm, and 28% of patients had lymph node involvement, Evans and colleagues found. On analysis, invasive size, histological grade, HER2 status, vascular invasion, tumor type, and mean stiffness were significantly associated with nodal involvement, Evans told session attendees.
"High tumor stiffness at shear-wave elastography is an independent predictor of lymph node involvement in women with invasive breast cancer," he said. "Our data may prove helpful for clinicians deciding which patients could benefit from neoadjuvant therapy."
ABUS matches handheld
During the same session, Dr. Eunjeong Kim, of the Catholic University of Korea, presented research indicating that automated breast ultrasound (ABUS) has similar diagnostic performance to handheld ultrasound.
Kim and colleagues evaluated 42 patients with 43 breast lesions who had been scheduled for an ultrasound-guided or stereotactic biopsy for suspicious calcifications on mammography. Each patient underwent both ABUS and handheld ultrasound.
Of the 43 lesions, 25 were malignant (58.1%) and 18 were benign (41.9%). There was no significant difference in the area under the curve (AUC) between automated breast ultrasound and handheld ultrasound (0.758 compared to 0.786, respectively).
"Automated breast ultrasound detected 96% of the malignant calcifications that had been found on mammography," Kim said. "Detection was found to be related to the pathology, calcification extent, and shape at mammography."
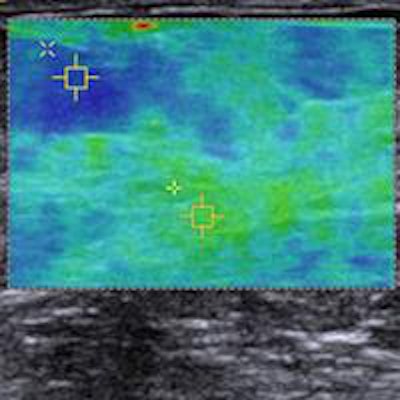
Editor's note: The image on the home page is a virtual touch tissue imaging quantification image of a healthy breast showing fatty tissue (1.38 m/sec) and parenchyma (3.33 m/sec). Image courtesy of Dr. Michael Golatta.