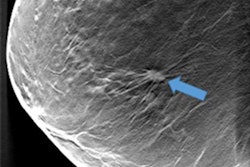
Adding 3D automated breast ultrasound (ABUS) to digital mammography in a screening setting significantly improves the invasive breast cancer detection rate in women with dense breasts and results in an acceptable recall increase, Swedish researchers have found.
The study evaluated the effect of adding 3D ABUS to full-field digital mammography (FFDM) for asymptomatic women with dense breasts. Researchers at the high-volume breast cancer screening mammography center performed FFDM followed by ABUS. The research team, led by Dr. Brigitte Wilczek, PhD, from the breast imaging department at Unilabs Capio Sankt Görans Hospital in Stockholm, found that 3D ABUS is well-suited for the screening workflow, increases cancer detection, maintains an acceptable recall rate, and doesn't add to radiation dose.
"Our findings clearly show that it is feasible to implement 3D ABUS into a high-volume FFDM center and increase the cancer detection rate in women ages 40 to 74 years, while maintaining an acceptable low recall rate well within the recommendations of the European guidelines for quality assurance in breast cancer screening and diagnosis," the authors wrote in an article published in the European Journal of Radiology on 7 June.
Why ABUS?
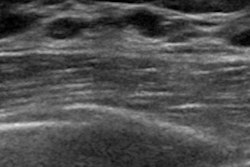
It is well-known that mammography is not as sensitive in women with dense breasts -- the sensitivity could be as low as 48%. Ultrasound has been suggested as an adjunct, but the traditional form -- handheld ultrasound -- is operator-dependent, time-consuming, and difficult to reproduce. Enter 3D ABUS, which has a standardized acquisition protocol and short training requirements, and can be evaluated in multiple planes. The modality also allows for reproducibility. But how does it hold up in a high-volume breast cancer screening center when added to FFDM? That's exactly what Wilczek et al sought to find out.
The researchers included 1,668 asymptomatic women ages 40 to 74 who had heterogeneously dense parenchyma (American College of Radiology, ACR 3) or extremely dense breasts (ACR 4). FFDM was performed using standard craniocaudal (CC) and mediolateral oblique (MLO) views followed by anteroposterior, lateral, and medial acquisitions of 3D ABUS (U-Systems) in both breasts.
All mammograms were double-read by two dedicated breast radiologists. The 3D ABUS exams were read by the first radiologist immediately after reading the mammograms. The second reader looked at 3D ABUS only if there was a need for consensus discussion because of unclear or abnormal findings.
What happened?
Adding ABUS to FFDM generated a total of 6.6 cancers per 1,000 women screened (p < 0.001), compared with 4.2 cancers per 1,000 women screened with FFDM alone.
In terms of recall, the rate was 13.8 per 1,000 women screened for FFDM alone and 22.8 for FFDM plus ABUS, yielding a difference of an additional 9.0 recalls per 1,000 women screened, which is in range of the European guidelines for quality assurance in breast cancer screening and diagnosis. Also, the recall rate compares favorably with the reported recall rate of 10.7% in the American College of Radiology Imaging Network (ACRIN) study and the 8.8% rate in the Japan Strategic Anticancer Randomized Trial (J-START), the researchers pointed out.
Additionally, adding 3D ABUS resulted in an increase in sensitivity of 36.4% compared with FFDM alone, and 25% when interval cancers were included in the analysis.
"One challenge in using 3D ABUS is the time needed to perform and examine the images," Wilczek and colleagues wrote. "In our study, the examination done by the radiographer took 15 minutes and the radiologist's interpretation of 3D ABUS five to seven minutes."
Other challenges include the fact that all dedicated breast radiologists involved in the study had to undergo tutorials prior to study initiation and familiarize themselves with ABUS, leading to individual learning curves.
Also, 3D ABUS was double-read only in case of discussions, while FFDM was always double-read. Furthermore, a computer-aided detection (CAD) system was not available for 3D ABUS, which could have helped reduce reading time and improve early cancer detection, they added.
Further studies in this area are needed, the researchers concluded. "In order to find the best strategies and methods to detect more breast cancers and reduce the number of investigated benign lesions, further studies are needed," they wrote.
Study disclosures
Financial support for this study was provided by U-Systems. However, funding sources had no involvement in the collection, analysis, and interpretation of data; in the writing of the article; or in the decision to submit the article for publication, according to the researchers.