The accuracy of 320-detector-row coronary CT angiography (CTA) combined with CT perfusion (CTP) is equivalent to that of SPECT myocardial perfusion for diagnosing functionally significant coronary artery disease, according to results of the prospective, multicenter, international CORE320 trial published in the European Heart Journal.
The accuracy of CTA for detecting flow-limiting disease was substantially improved with the addition of CT perfusion, wrote Dr. Carlos Rochitte, from the University of São Paulo Medical School in Brazil, and colleagues at 15 other centers in eight countries.
"CT perfusion when combined with CT angiography has a clear and undeniable benefit over CT angiography alone, compared with the most comprehensive reference standards published to date," co-author Dr. Frank Rybicki, from Brigham and Women's Hospital of Boston, said in an interview.
"The reference standard for a hemodynamically significant lesion is a lesion that's seen on catheterization that causes a perfusion abnormality on SPECT," he continued. "We put cath and SPECT together [with CTA-CTP] so you could actually say for sure that the lesion was hemodynamically significant."
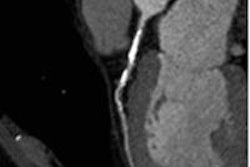
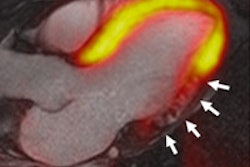
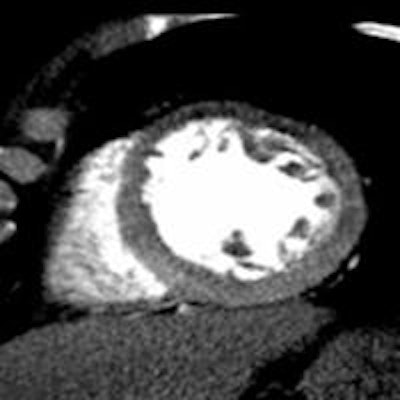
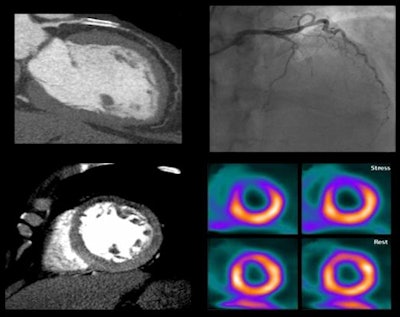 Image of CORE320 patient shows an occluded left anterior descending (LAD) stent on CT and catheterization, with the corresponding anterior wall defect demonstrated by CT perfusion and SPECT. Image courtesy of CORE320 investigators.
Image of CORE320 patient shows an occluded left anterior descending (LAD) stent on CT and catheterization, with the corresponding anterior wall defect demonstrated by CT perfusion and SPECT. Image courtesy of CORE320 investigators.The value of CT perfusion
Both invasive coronary angiography and CTA provide morphologic data, but they lack the physiologic information needed to determine the hemodynamic significance of a lesion. Proving that functional significance requires either catheter-based fractional flow reserve techniques, or noninvasive modalities such as SPECT myocardial perfusion imaging (MPI), PET, or MRI, the authors explained (Eur Heart J, November 19, 2013).
Previous studies performed in one or two centers have demonstrated the value of CT perfusion combined with CTA, but the results have not been compared with comprehensive reference standards, Rybicki said. As a result, CORE320 was designed to test the hypothesis that noninvasive CTA-CTP could reliably detect or exclude the presence of flow-limiting coronary stenoses in patients with suspected coronary artery disease (CAD), using a strong composite reference standard of invasive coronary angiography plus SPECT/MPI.
The study examined hemodynamically stable patients (age, 45 to 85 years) with suspected or known CAD but without contraindications to CTA who were referred for conventional angiography. The team examined 381 patients at 16 centers using CTA and adenosine stress CTP, SPECT/MPI, and conventional coronary angiography. A full clinical history and physical exam were also obtained.
The noninvasive imaging exams were performed prior to invasive angiography in a CORE320-validated laboratory, the authors explained. SPECT could be performed with either exercise or pharmacologic stress.
The CT images were acquired using a protocol developed for the 320-detector-row CT scanner (Aquilion One, Toshiba Medical Systems), following administration of beta-blockers, sublingual nitrates, and 50 to 70 mL of iodinated contrast. Contrast was injected at 4 to 5 mL/sec for each of the axial electrocardiogram-triggered acquisitions. CTP was acquired during a continuous six-minute infusion of adenosine.
Independent core laboratories reconstructed and interpreted sinograms for all scans, and the labs performing CTA and CTP were blinded to the results of each other's tests, the authors wrote. At CTA, all lesions with 30% or greater stenosis underwent quantitative evaluation using a Vitrea fX workstation (Toshiba).
For detecting or excluding flow-limiting coronary artery disease, combined CTA-CTP showed an area under the curve (AUC) of 0.87 for all patients. In patients without prior myocardial infarction, AUC was even higher at 0.90, and in patients without any prior coronary artery disease, AUC was 0.93. For a patient with 50% or greater stenosis and a perfusion deficit at CTP, the sensitivity and specificity of CTA-CTP were 80% and 74%, respectively.
Meanwhile, the prevalence of obstructive CAD defined by angiography and SPECT was 38%; by angiography alone, prevalence was 59%. The median radiation dose was 11 mSv for the combined CTA-CTP tests, according to Rybicki, who said that detailed radiation exposure results will be available in an upcoming publication.
Combined CTA-CTP underestimated coronary artery disease in 29 patients (false-negative results) and overestimated CAD in 61 patients (false-positive results), compared with the combined outcome of angiography and SPECT, the group reported.
"There is no significant difference between doing this noninvasively and using the reference standard," said Rybicki. "There is clear and undeniable evidence that this strategy works to stratify lesions."
The method didn't work quite as well in patients with previous myocardial infarction. Patients without a prior infarction somehow seem to have "a cleaner CT perfusion" and were more easily diagnosed, he said. Excluding patients with prior myocardial infarction increased the diagnostic power of combined CTA-CTP in the noninvasive detection of flow-limiting CAD.
Which technique is best?
In the constellation of noninvasive CT alternatives for determining the functional significance of a lesion -- one that includes fractional flow reserve CT (FFR-CT) -- is one technique emerging as a better choice to determine the functional significance of lesions? There is plenty of research left to do in that arena, Rybicki said.
"CT with gradients is a potential game changer, FFR-CT is a potential game changer, CT perfusion is a potential game changer -- and all of them work," he said. "Each method is different, but they're all trying to use CT for the next iteration of cardiac CT, which is to assess function. The question is which one is the right test and the most cost-effective test for each type of patient. And that is going to be a part of the evolving landscape of doing CT for the heart."
That said, there are certain efficiencies inherent in performing CTA and CTP at the same time (rather than having FFR-CT analyzed in a lab after CTA is completed, for example) that could give CTA-CTP an edge, at least among certain patient groups.
How about equipment? Wouldn't it be possible to do the same CTA-CTP scans on, say, a dual-source CT scanner? It would, Rybicki said, but 320-detector-row technology offers less variability in contrast enhancement because it images the heart in a single beat.
"For perfusion CT, 320 is the best technology because it uniformly images the heart and you don't have to worry about contrast," he said, cautioning that it was his opinion and not the conclusion of any study to date. But it makes sense in theory, he added.
In the old days, coronary CTA was just a matter of opacifying the coronary arteries. But with today's shift from pure morphologic imaging to real functional imaging, "it becomes a question of contrast enhancement," Rybicki said. "You want to see the subtle differences in enhancement in the myocardium, you want to be able to measure flow, and you want to be able to do viability."
Study disclosures
The study was funded by Toshiba. Study data were strictly controlled by the authors in the core labs, according to Rochitte and colleagues.