Using breast MRI to estimate tumor size in high-risk patients is comparable to the modality's performance for sporadic cancers. This means breast MRI can safely be used for treatment planning, Dutch researchers believe.
Breast MRI is a known screening modality for women with a high risk of developing breast cancer -- namely BRCA1 or 2 carriers, and those with a family history. Breast MRI is usually combined with mammography for detecting microcalcifications, but treatment decisions are nowadays largely based on MRI findings, noted Dr. Ritse Mann from Radboud University Nijmegen Medical Centre in the Netherlands and colleagues (European Journal of Radiology, 5 April 2013).
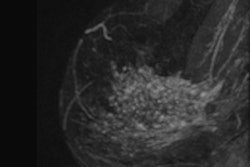
"This seems deservedly so, as studies have repeatedly shown that tumor size estimation with MRI is much better than with mammography," they wrote. "This holds especially true in women with dense breasts and those developing invasive lobular carcinomas. Moreover, breast MRI tends to detect carcinomas in an earlier stage than mammography, and many carcinomas are not even visible on mammography."
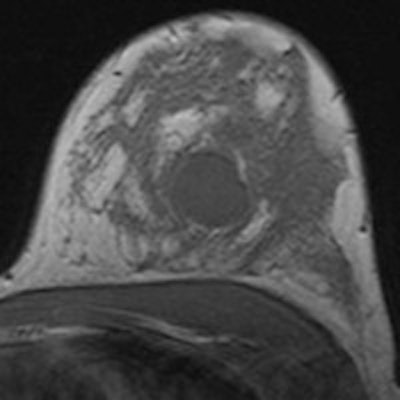
However, the accuracy of breast MRI for staging purposes has only been tested in sporadic cancers. The researchers sought to assess the quality of tumor size estimation using MRI in high-risk patients for the whole tumor area (including invasive carcinoma and ductal carcinoma in situ [DCIS]) and the largest focus (in the subset of patients with invasive carcinomas). They also sought to assess whether differences in the quality of size estimation among BRCA1, BRCA 2, and non-BRCA-carrier patients are present.
Mann and colleagues assessed concordance of radiologic staging using MRI with histopathology in 49 tumors in 46 high-risk patients (23 BRCA1, 12 BRCA2, and 11 non-BRCA patients). The size of the total tumor area (TTA) was compared with pathology. In invasive carcinomas (n = 45), the size of the largest focus (LF) also was addressed.
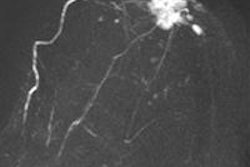
The researchers found correlation of MRI measurements with pathology was 0.862 for TTA and 0.793 for LF. TTA was underestimated in eight (16%), overestimated in five (10%), and correctly measured in 36 (73%) cases. LF was underestimated in four (9%), overestimated in five (11%), and correctly measured in 36 (80%) cases. Impact of BRCA1 or 2 mutations on the quality of size estimation was not observed.
There is reasonable agreement of MRI-determined tumor sizes with histopathologic findings in high-risk patients. MRI strongly outperformed mammography, both in sensitivity and tumor size estimation, the researchers found.
The presence or absence of a BRCA1 or BRCA2 mutation didn't appear to be strongly related to failures of tumor size estimation, nor are BRCA-related tumors better measured than sporadic tumors.
"The poor correlation of the radiologically assessed total tumor area with pathologic size in BRCA2 carriers is a striking exception, but must be interpreted with caution due to the low number of BRCA2 carriers in our study," they added.
The most influential factor for failure of adequate tumor size estimation is the pathologic T-score. There was a clear risk of tumor size underestimation in larger cancers. This implies tumors with a lot of surrounding DCIS are less accurately measured than tumors with only a limited DCIS fraction.
"Moreover, the quality of tumor size estimation is dependent on the appearance of a tumor at MRI, and is worse in nonmass-like enhancing lesions than in clear masses. Our results are in line with reported MRI-pathology correlations in women without specific high-risk profile that are usually calculated by correspondence of the largest focus with the largest invasive tumor at pathology although this is often not specifically mentioned," they wrote.
There is "surprisingly little" reported in the literature on the causes of under- and overestimation of tumor size on MRI compared with pathology, even though many papers on the correlation of size have appeared, according to the authors.
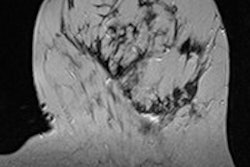
The shape of the breast at both examinations may be a contributing factor. On MRI, the breast hangs freely within the loops of the breast coil; at pathology, the simple mastectomy specimen or lumpectomy specimen is flat on the table. Thus, the left-to right and cranial-to-caudal diameter of the breast at pathology is larger than at MRI, while the anterior-posterior diameter decreases.
Another factor may be MRI features of the breasts such as moderate to marked background enhancement and neovascularization just outside of the pathologic tumor area. Some precursor lesions such as atypical ductal hyperplasia and lobular carcinoma in situ may enhance, but are not included within the pathologic total tumor area.
Underestimation of tumor size is most likely due to small satellite foci that do not show enhancement. In Mann and colleagues' study, breast specimens were examined in a more standard way with specimen radiographs and extensive tissue sampling.
"However, we observed underestimation of the total tumor area with more than 1 cm in only 10% of cases," he wrote. "Consequently, many of these occult foci occur apparently within the MRI visible total tumor area and will therefore be correctly treated when the treatment plan is based on the MRI."
At least some tumor foci may escape detection on both MRI and in standard pathologic analysis, but the importance of these occult satellite foci for surgery is questionable, he added.
Despite the less than perfect concordance of MRI with pathologic findings, "treatment decisions in high-risk patients can safely be made on the basis of MRI findings," the researchers concluded. "Obviously, it remains essential to inform patients about the risks of tumor size under- and overestimation that nevertheless exist."