Before preoperative breast MRI, it's feasible to work out which patients are most likely to show similar results on mammography and ultrasound, and this may help to save on the expense of an MRI exam, Dutch researchers have found.
Controversy persists over the role of contrast-enhanced MRI of the breast in patients with known breast cancer and eligible for breast-conserving therapy (BCT), explained Kenneth Pengel, a PhD candidate from the department of radiology at the Netherlands Cancer Institute, Amsterdam, and colleagues from the Utrecht University Medical Center.
Several studies have demonstrated that MRI has superior sensitivity to detect invasive breast cancer compared with mammography and ultrasound as well as clinical breast examination (CBE), and this sensitivity leads to improved definition of tumor extent.
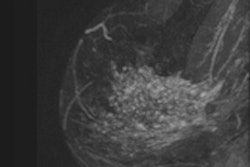
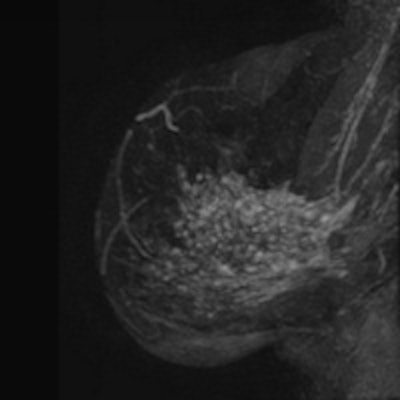
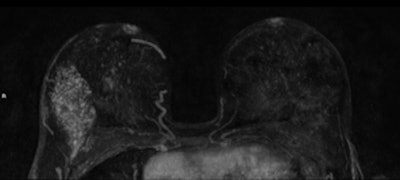 A 45-year-old woman with invasive lobular carcinoma (ILC) in her right breast shown as heterogeneous segmental nonmass enhancement of 75 mm on preoperative breast MRI (axial and sagittal maximum intensity projection). The ILC was mammographic occult and only 8 mm on ultrasound. After pathological proof of the more extensive size, the treatment was altered to mastectomy. All images courtesy of Kenneth Pengel and Dr. Claudette Loo.
A 45-year-old woman with invasive lobular carcinoma (ILC) in her right breast shown as heterogeneous segmental nonmass enhancement of 75 mm on preoperative breast MRI (axial and sagittal maximum intensity projection). The ILC was mammographic occult and only 8 mm on ultrasound. After pathological proof of the more extensive size, the treatment was altered to mastectomy. All images courtesy of Kenneth Pengel and Dr. Claudette Loo.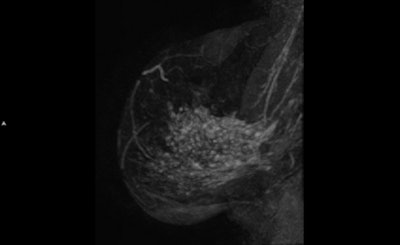
"As a result, MRI has been expected to increase complete resection rates, breast cancer control, and cosmetic outcome, but these effects have not been demonstrated consistently," they noted in an article published online on 27 October by the European Journal of Radiology.
Therefore, the group sought to determine when preoperative breast MRI will not be more informative than available breast imaging and can be omitted in patients eligible for BCT. They performed an MRI exam in 685 consecutive patients with 692 invasive breast tumors and eligible for BCT based on conventional imaging and clinical examination. They explored associations between patient, tumor, and conventional imaging characteristics and similarity with MRI findings.
The cohort consisted of women with invasive breast cancer who participated in the MARGINS (Multimodality Analysis and Radiogical Guidance IN breast conServing therapy) study conducted at the Netherlands Cancer Institute between 2000 and 2008. In the MARGINS study, women with pathology-proven invasive breast cancer and eligible for BCT on the basis of conventional imaging and CBE were consecutively recruited for an additional preoperative breast MRI, the authors pointed out. Before MRI, all patients underwent conventional imaging and CBE, and proof of malignancy was obtained by means of fine needle aspiration cytology (FNAC) and/or a core biopsy.
Initially, mammography was carried out on a Trex LORAD MIV systems or a Philips Healthcare Mammo Diagnost 3000 unit, using Agfa Healthcare HDR films. In 2004, the institute switched to digital mammography: Selenia, from Hologic. Both breasts were imaged in the cranio-caudal and medio-lateral oblique directions. Ultrasound was performed with a Kretz Voluson V730 (Kretztechnik) or a Philips IU22 system. Ultrasound of the axilla was performed in all patients and an FNAC was done for proof of malignancy of suspicious lymph nodes. MRI exams were performed initially using a 1.5-tesla scanner (Magnetom, Siemens Healthcare), and from April 2007 using a 3-tesla scanner (Achieva, Philips Healthcare).
The mean age of the women was 56.6 years (standard deviation 10.4 years). The majority (76.5%) had invasive ductal cancer (IDC) and 20% had invasive lobular cancer (ILC). Additional malignant disease on MRI (i.e., discordant findings with conventional imaging) was detected in 107 of the 692 breasts (15.5 %). Of the 237 tumors with postoperative positive lymph nodes, 54 (22.8%) were detected preoperatively by ultrasound and subsequent FNAC.
At univariate analysis, age, preoperative lymph node positivity (FNAC), HER2-positivity, discrepancy in tumor diameter between mammography and ultrasound (including mammographic occult), and presence of ILC were significantly associated with discordant findings (p < 0.001, p = 0.011, p = 0.044, p = 0.001, p = 0.005, respectively). At multivariate analysis these factors, except HER2-positivity, retained significance. The area under the ROC curve was 0.68, 95% confidence interval: 0.63-0.74. Discrepancy in tumor diameter between mammography and ultrasound occurred significantly more often in younger patients and patients with breast density ACR 3 and 4 (p < 0.001).
A significant association was found between discordant malignant findings and postoperative lymph node status (p < 0.001). Contralateral breast cancer on MRI was detected in five of the 685 patients (0.7%). These cancers, which were occult at conventional diagnosis, were not included in the analysis as discordant malignant findings, according to the authors.
"There is similarity between conventional imaging and MRI in approximately 85% of BCT patients. So regardless which guidelines are used for preoperative breast MRI, the value of this technique can be disputed in this group of patients," they wrote. "If this group could be identified prior to the decision to perform the MRI, studies on MRI-detected additional disease could be powered more efficiently while reducing the number of clinical procedures and cost."
Some developments may have affected the study, however. Digital mammography was implemented during the study period, and this improved imaging technique may lead to the detection of more lesions and consequently more similar findings with MRI. Also, the transition from a 1.5-tesla to a 3-tesla MRI unit took place; the rate of similar findings using the 1.5-tesla unit was 84.7% and 87.7% with the 3-tesla machine.
Finally, from 2004 onwards, patients with preoperatively proven positive lymph nodes were gradually referred to a neoadjuvant chemotherapy study. This change in policy may have led to an underestimation of the impact of preoperative lymph node status on the rate of discordant findings.
"Our research is mainly focused on several applications of breast MRI: preoperative staging, monitoring during neoadjuvant chemotherapy. In collaboration with the nuclear medicine department, we are currently investigating the role of PET/CT and MRI combined to predict response to neoadjuvant chemotherapy," Pengel noted in an email to AuntMinnieEurope.com.
The study was financially supported by the Dutch Cancer Foundation. Dr. Claudette Loo, a breast radiologist, was the second author of the EJR article.