
The posteroanterior (PA) chest radiograph remains a powerful tool in diagnosing mediastinal diseases, but to detect an unsuspected mass and avoid potential mistakes, it's essential to understand the concept of mediastinal reflections, according to prize-winning research.
Despite the 2D representation of mediastinal structures, PA chest x-rays can still be used to localize the detected abnormalities in the anterior, middle, or posterior mediastinum, noted Dr. Nadežda Bystrická, from the department of radiology, Národný Onkologický ústav, Bratislava, Slovakia. Along with colleagues Dr. Hana Poláková and Dr. Juraj Sýkora, she received a certificate of merit for her e-poster presentation at ECR 2013.
The group reported these mediastinal reflections can be identified with conventional radiography:
Mediastinal lines: Thin (< 1 mm wide), linear opacities resulting from contact between two aerated structures surrounding thin intervening tissue on both sides, such as the anterior and posterior junction lines.
Mediastinal stripes: Bands that result from air surrounding thicker intervening mediastinal structures. The mediastinal stripes present on PA chest radiographs include the right and left paratracheal stripes.
Mediastinal interfaces: Edges, which are produced by contact between the aerated lung and adjacent mediastinal structures. The mediastinal interfaces include the right and left paraspinal lines, the azygoesophageal recess, the aortic pulmonary stripe, the para-aortic line, and cardiac borders.
The frequency of these reflections on chest radiographs is variable, and is shown in table 1, they stated. The absence of one of the mediastinal lines, stripes, or interfaces can be insignificant because it may be caused by anatomic variations or by technical conditions, but the presence, obliteration, thickening, or distortion of these lines, stripes, and edges can reveal mediastinal disease.
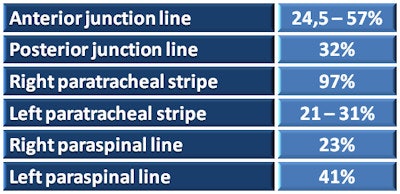 Table 1: Frequency of visualization of different mediastinal reflections on frontal chest radiographs. Source: Radiology department, Národný Onkologický ústav, Bratislava.
Table 1: Frequency of visualization of different mediastinal reflections on frontal chest radiographs. Source: Radiology department, Národný Onkologický ústav, Bratislava.Furthermore, these findings can be used to localize mediastinal masses in the anterior, middle, or posterior mediastinum (see table 2), and therefore may help to narrow the differential diagnosis and determine the most appropriate further diagnostic workup.
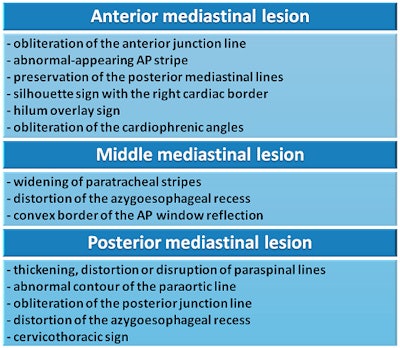 Table 2: Radiographic findings that help localize a mediastinal lesion within the anterior, middle, or posterior mediastinum. Source: Radiology department, Národný Onkologický ústav, Bratislava.
Table 2: Radiographic findings that help localize a mediastinal lesion within the anterior, middle, or posterior mediastinum. Source: Radiology department, Národný Onkologický ústav, Bratislava.The normal radiographic appearance of the anterior junction line is as a thin oblique line projecting over the superior two-thirds of the sternum and runs from the upper right to the lower left. It does not extend above the level of clavicles. It may be absent when its course is not tangential to the x-ray beam, and it can be obscured by other structures such as the heart, great vessels, or the thoracic spine.
"Obliteration or abnormal convexity suggests anterior mediastinal disease, although it is usually the preservation of more posterior lines at radiography that helps identify the location of an anterior mediastinal mass. Displacement of the line may be due to hyperinflation or volume loss of the surrounding lung," Bystrická wrote.
The normal radiographic appearance of the posterior junction line is as a thin straight line projecting through the trachea. Unlike the anterior junction line, it can be seen above the clavicles. Abnormal bulging, convexity, or obliteration of this line suggests a posterior mediastinal abnormality, and further clues to the location of a mass can be inferred from the lateral margins of the mass above the clavicles, she explained.
The right paratracheal stripe begins at the level of the clavicles and extends inferiorly, projecting through the superior vena cava, to the right tracheobronchial angle at the level of azygos arch. This stripe has a maximum normal thickness of 4 mm, and it should be uniform in width. An abnormal contour, widening, or obliteration of this stripe may be due to abnormality of any of its components, from the tracheal mucosa to the pleural space, such as tracheal carcinoma, paratracheal masses (most commonly lymphadenopathy), and pleural effusion or thickening, according to the researchers.
The left paratracheal stripe extends superiorly from the aortic arch to join with the reflection from the left subclavian artery. It may be obscured by contact between the left upper lobe and either the proximal left common carotid artery anteriorly or the left subclavian artery posteriorly (i.e. by the pararterial line). An abnormal contour or widening may be caused by pleural effusions or thickening, paratracheal lymphadenopathy, hematomas, or neoplasm.
On a frontal radiograph, the aortopulmonary (AP) window reflection extends from the aortic knob to the left pulmonary artery. This should have a concave or straight border, but a straight contour should be considered abnormal if previous studies demonstrated a concave border, they added. A convex shape of the AP window reflection is considered abnormal. The abnormal convexity of the AP window reflection may be due to middle mediastinum abnormalities such as lymphadenopathy, bronchial artery aneurysms, nerve sheath tumors, bronchopulmonary foregut malformations, or prominent mediastinal fat.
The AP stripe extends from the aortic arch to the level of the left main bronchus, where it usually continues as the border of the left side of the heart. It delineates the anterior margin of the AP window and is normally straight or slightly convex. The normal appearance of this interface may be altered by anterior mediastinal disease such as thyroid masses, thymic tumors, and lymphadenopathy.
The azygoesophageal recess is seen on a frontal radiograph as a vertically oriented interface. In its upper third, it may be straight or show mild leftward convexity. Right superior convexity may be seen in children and younger adults. The middle third of the recess may be the most variable in the appearance, but typically it is straight edged or demonstrates mild leftward convexity. In its lower third, it usually appears as a straight edge.
"Abnormal contour, convexity, or disappearance of this interface suggests disease affecting the middle and posterior mediastinal compartments such as lymphadenopathy, bronchopulmonary-foregut malformations, pleural abnormalities, left atrial enlargement, esophageal disease, and hiatal hernia," the authors noted.
The right paraspinal line appears straight and runs from the eighth through the 12th thoracic vertebral levels. The left paraspinal line runs vertically from the aortic arch to the diaphragm and lies medial to the para-aortic line, although sometimes it can lie lateral to the para-aortic line. The paraspinal lines may be displaced laterally by prominent mediastinal fat or osteophytes. Abnormal contour or displacement may also suggest posterior mediastinal disease such as mediastinal hematoma, mass, or extramedullary hematopoiesis, they reported.
The para-aortic line appears as a straight vertical interface, which lies posterior to the cardiac shadow and lateral to the left paraspinal line. In its lower third it comes nearer to the vertebral bodies at the level of the 11th thoracic vertebra, overlapping the left paraspinal line. An abnormal contour may be the result of different conditions affecting the lung and pleura or the middle and posterior mediastinum, such as lymphadenopathy, aortal aneurysm, gastroesophageal varices, and lung neoplasms.
Editor's note: The image on the home page is courtesy of Craig Moore, a physicist and radiation protection adviser at Queen's Centre for Oncology and Haematology at Castle Hill Hospital in Cottingham, U.K.



















