
Despite the increasing use of CT for identifying mediastinal abnormalities, the chest x-ray remains a valuable tool in the evaluation of the mediastinum, and in many cases frontal and lateral chest radiographs remain the first diagnostic examination performed for lung and mediastinal evaluation, say researchers from Portugal.
"The chest radiograph presents a considerable amount of useful information. Evaluation of the anatomy of the mediastinum, including mediastinal lines, stripes, and spaces, provides important hints and may point out the need for further investigation," noted radiology resident Dr. Henrique Donato and colleagues from the faculty of medicine at the University Hospital of Coimbra in Portugal. "Due to the extreme frequency of the chest radiograph, it is important to recognize mediastinal abnormalities in this imaging modality. In order to do so, it is essential to be familiar with the normal radiographic appearance."
Knowledge of normal radiographic mediastinal anatomy is pivotal for detection of abnormalities, they stated in an e-poster presentation at last month's ECR 2014 in Vienna.
The mediastinum is often divided into compartments, but these divisions are theoretical, with no physical boundaries to limit disease, according to Donato and colleagues. The modified anatomic division is one of the most popular methods of division of the mediastinum (see table). Identifying the involved compartment can direct the investigation and narrow the differential diagnosis, and evaluation of the mediastinal lines and recognition of radiographic signs aid in the localization of abnormalities.
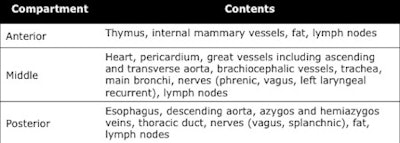 Contents of the mediastinal compartments. Source: Dr. Henrique Donato, Faculty of Medicine of Coimbra, Portugal, presented at ECR 2014.
Contents of the mediastinal compartments. Source: Dr. Henrique Donato, Faculty of Medicine of Coimbra, Portugal, presented at ECR 2014.The authors' prime aims were to review the radiological anatomy of the mediastinum and the normal appearance of mediastinal lines, stripes, and spaces, and to recognize signs on the chest radiograph that aid in the evaluation of mediastinal abnormalities. They provided the following checklist of key points to remember:
Mediastinal lines, stripes, and spaces, which are formed by the anatomic relations between the lungs, mediastinum, and pleura. Although their visibility and significance vary, they are valuable in the assessment of specific mediastinal structures and compartments.
Anterior junction line. This is the anterior region of contact between the lungs with a variable amount of intervening fat. Normal radiographic appearance: crosses obliquely the superior two-thirds of the sternum, from upper right to lower left, with a superior V-shaped recess. Abnormal appearance: obliterated by anterior mediastinal disease, displaced by unilateral lung volume changes.
Cardiophrenic angles (i.e., junction of the right and left heart borders with the diaphragm, in the anterior mediastinum). Normal radiographic appearance: concave. Abnormal appearance: epicardial fat pad, pericardial cyst, lymphadenopathies, other anterior mediastinal masses.
Right paratracheal stripe. This is the region of contact between the right lung and the right tracheal wall, with intervening mediastinal fat, and probably is the most commonly seen mediastinal line. Normal radiographic appearance: width less than 5 mm. Abnormal appearance: tracheal and pleural abnormalities, lymphadenopathies.
Vascular pedicle, which corresponds to the transverse width of the upper mediastinum, measured from the superior vena cava interface to the left subclavian artery interface. Normal radiographic appearance: width ≤ 58 mm. Abnormal appearance: dilatation of the great vessels, lymphadenopathies, mediastinal mass, or infiltration and pleural abnormalities.
Posterior junction line (posterior region of contact of the lungs, between the esophagus and the thoracic spine, with variable amounts of intervening fat). Normal radiographic appearance: vertical line or stripe projecting through the trachea, above the level of the anterior junction line.Abnormal appearance: obliterated by posterior mediastinal disease, displaced by unilateral lung volume changes.
Aortopulmonary window, which is the mediastinal space limited superiorly by the aortic arch, inferiorly by the pulmonary artery, medially by the trachea and esophagus, and laterally by the lung. It contains fat, lymph nodes, the left laryngeal recurrent, and left phrenic nerves. Normal radiographic appearance: normally concave or straight. Abnormal appearance: lymphadenopathies, accumulation of fat, aortic aneurysm.
Azygoesophageal recess. This is the interface between the retrocardiac mediastinum (esophagus anteriorly, azygos vein posteriorly) and the right lower lobe. Normal radiographic appearance: line with a shallow reverse C or reverse S shape, extending from the azygos vein arch to the diaphragm. Abnormal appearance: lymphadenopathies, foregut cysts, left atrial dilatation or esophageal disease, including hiatal hernia.
Para-aortic line, or interface between the descending aorta and the left lung in the posterior mediastinum. Normal radiographic appearance: vertical line, parallel and generally external to the left paravertebral stripe. In the lower third, it may overlap with the left paravertebral stripe. Abnormal appearance: vascular aortic disease, posterior mediastinal masses. This line can be displaced in the elderly.
Paravertebral stripes (interfaces between the lungs and the paravertebral fat and soft tissues). The left stripe is more commonly seen, because the aorta promotes a more tangential interface to the x-ray beam. Normal radiographic appearance: vertical lines, parallel to the spine. Abnormal appearance: posterior mediastinal abnormalities, such as neurogenic tumors or extramedullary hematopoiesis. Also, decubitus, prominent mediastinal fat, osteophytes.
Retrosternal stripe. This is formed by the contact of the lungs and the retrosternal soft tissues, and contains the internal mammary vessels and lymph nodes. Normal radiographic appearance: stripe located posterior to the sternum on the lateral projection. Normal thickness up to 7 mm. Abnormal appearance: sternal, internal mammary vessel and lymph-node abnormalities.
Retrosternal clear space (region containing the thymus and retrosternal tissues). Normal radiographic appearance: lucent area seen on the lateral projection, posteriorly to the sternum and anteriorly and superiorly to the heart and great vessels. Abnormal appearance: increased in emphysema; decreased in heart or great vessel enlargement, anterior mediastinal mass.
Posterior tracheal stripe, which corresponds to the posterior tracheal wall and sometimes the esophagus, outlined posteriorly by air in the lung or esophagus. Normal radiographic appearance: variable length and thickness. Abnormal appearance: esophageal carcinoma, tracheal wall thickening.
Finally, Donato et al also urged radiologists to keep aware of the following radiographic signs:
Silhouette sign. An intrathoracic lesion that is contiguous with a mediastinal structure or diaphragm and has the same density will obliterate that structure's border. The presence or absence of this sign allows identification and localization of mediastinal lesions.
Hilum overlay sign. If the hilar vessels are clearly seen through a mass projecting over the hilar region, it means that the mass is either anterior or posterior to the hila.
Cervicothoracic sign, which is based on the fact that the anterior mediastinum ends at the level of the clavicles, whilst the posterior compartment extends more superiorly. A mass clearly visible above the clavicles must be intrathoracic and posterior, they concluded.



















