The risk and incidence of contrast-induced nephropathy (CIN) may be overestimated, according to an eminent group of Danish researchers led by Dr. Henrik Thomsen. Patients can have natural fluctuations in their S-creatinine levels because estimated glomerular filtration rates (eGFR) vary regardless of whether a patient received contrast or not, they suggest.
Many factors can affect the S-creatinine level in a patient, including illness, hydration, food, muscle mass, and medications, according to Thomsen, professor of radiology at the University of Copenhagen and former president of the European Society of Urogenital Radiology (ESUR).
 Dr. Henrik Thomsen, University of Copenhagen.
Dr. Henrik Thomsen, University of Copenhagen.
CIN is a diagnosis based on the presence of an increase in S-creatinine levels and is a diagnosis of exclusion, he told delegates at ECR 2014 in Vienna.
"We don't have confirmation that it is really contrast-induced nephropathy," he said.
To understand whether fluctuations in S-creatinine levels are caused by the contrast medium or other factors, a control group who did not receive contrast is important, he added.
Thomsen and colleagues constructed a study of fluctuations in eGFR in relation to contrast-enhanced CT and MRI compared with outpatient control groups. eGFR was determined before the imaging procedure and three days later at the department or the patient's home. The iodine-and gadolinium-based contrast media were the same as used for all other exams in their department.
A total of 716 patients completed the study. The breakdown of patients with and without contrast medium (CM) was as follows:
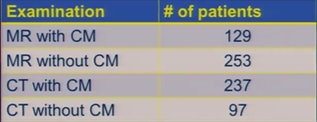 Chart courtesy of Dr. Henrik Thomsen.
Chart courtesy of Dr. Henrik Thomsen.The researchers found a statistically significant but not clinically relevant rise in eGFR after three days in all four groups, Thomsen reported. The average eGFR variation was 4.8 mL/min/1.73 m2.
They found large variations in eGFR between the two measurements in 41% of the patients, as they had a change greater than ± 10 mL/min/1.73 m2. Only three patients fulfilled the CIN requirement when the definition of S-creatinine of 44 µmol/L or more was used.
The relative definition was a different story:
| Contrast-enhanced MRI (n = 129) |
Unenhanced MRI (n = 253) |
Contrast-enhanced CT (n = 237) |
Unenhanced CT (n = 97) |
|
| CIN (S-creatinine ≥ 25%) |
13 (10.1%) | 33 (13.0%) | 13 (5.5%) | 8 (8.4%) |
"Similar fluctuations in eGFR occurred independently of whether the patient had contrast medium intravenously or not, and there were no differences between iodine- and gadolinium-based contrast media," Thomsen said.
The results probably reflect the natural variations in S-creatinine levels and the team's findings in outpatients are in accordance with the few other studies involving inpatients, he concluded.
In terms of daily clinical practice, Thomsen said radiologists should not be as strict as they currently are, but he's still concerned about patients because other studies focusing on this topic only included contrast-enhanced CT.
"I think it's correct that we have lowered the threshold of CIN to 45, maybe we can go down [even further]," he said.
Mostly, more studies are needed.
Thomsen and colleagues also recently published a study on this topic in the European Journal of Radiology (24 February 2014, article in press).