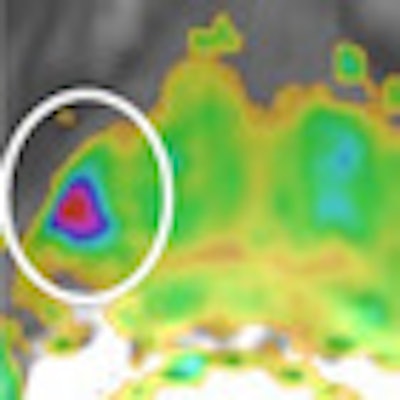
Diffusion-weighted imaging (DWI) is a powerful noninvasive imaging method that can provide useful qualitative and quantitative information about tumor cellularity and tissue structure in prostate cancer, and permits detecting and staging prostate carcinoma, noted a Spanish team in prize-winning research presented at ECR 2013.
DWI used in conjunction with T2-weighted MRI improves the detection of local recurrence after radiotherapy, hormonal therapy, or radical prostatectomy, and the technique facilitates the detection of lymph node and hematogenous metastasis in bone and liver. Also, it may be a useful tool to monitor the therapeutic effects of prostate cancer after hormonal and radiation therapy and for guiding targeted biopsies in patients with previously negative biopsy results, according to lead author Dr. Manuel Recio Rodríguez, a radiologist from Jefe Asociado del Servicio de Radiodiagnóstico del Hospital Universitario Quirón, Pozuelo de Alarcón, Madrid.
A pretreatment combination of apparent diffusion coefficient (ADC) values, Gleason score, and baseline prostate-specific antigen (PSA) levels may play an important role in risk staging for prostate cancer treatment, which can improve cancer control while reducing the risks of treatment-related complications. This could lead to a major extension in the role of MRI in tumor detection and staging in prostate cancer, reckoned the authors, who received a Magna Cum Laude award for their e-poster at the Vienna congress.
DWI has been applied to extracranial sites since the 1990s, but the advent of echo-planar imaging (EPI), high-gradient amplitude and multichannel coils, and parallel imaging have led to fewer motion artifacts and high-quality prostate images. The acquisition time of DWI in the prostate is relatively short, and it does not need the administration of contrast media, so DWI can be included easily in routine imaging protocols, they stated.
"DWI depends on the microscopic mobility of water. This mobility, classically called Brownian motion, is due to thermal agitation and is dependent on the cellular environment of water," the authors noted. "Bulky fluids in the body, such as the urinary bladder or gallbladder, show free and isotropic diffusion. In biologic tissues, however, water diffusivity is restricted by different components, such as tissue cellularity, tissue organization, extracellular space tortuosity, and the integrity of cell membranes."
This means diffusion-weighted MRI can provide information that reflects tissue cellularity and the integrity of cellular membranes. An echo-planar sequence is used for diffusion-weighted image acquisition, and is especially susceptible to magnetic field heterogeneities, although the use of an echo-planar sequence in abdominal imaging is particularly challenging due to the presence of air within the gastrointestinal tract and lung bases, they explained.
Other sources of susceptibility artifacts include medical devices (e.g., metallic stents, surgical clips) and grafts. One way to reduce susceptibility artifacts is to shorten the echo time and increase the bandwidth. To reduce such artifacts on a 3-tesla system, they recommend applying parallel acquisition image techniques that can reduce the echo time (TE) and the number of echoes, as well as increase bandwidth. A 3-tesla MR unit increases the signal-to-noise ratio (SNR) and makes it possible to use high values of b (> 1,000 s/mm2) and smaller slice thickness (# 3 mm).
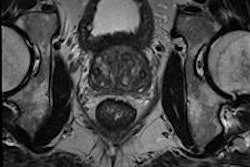
At their institution, the researchers perform prostate MRI using a 3-tesla MRI system (HDxt 3.0T, GE Healthcare) equipped with an eight-channel torso phased-array coil. "DWI is part of the routine prostatic MRI protocol. DW images are obtained by applying a single-shot echo-planar imaging sequence with the same slice location as the T2 sequences," they wrote.
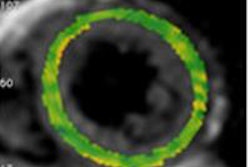
DWI and ADC have become powerful indicators for characterization of prostate tissue, particularly in differentiating between benign and malignant lesions. Healthy prostate tissue exhibits signal loss, whereas areas of restricted molecular motion, such as in densely packed tumor cells, show less signal loss and are therefore bright on the raw DWI, they continued. The signal intensity observed depends on both water diffusion and the T2 relaxation time. An area with a very long T2 relaxation time may remain high signal at DWI and be mistaken for restricted diffusion. This is known as the "T2 shine-through effect." A simple solution to this problem is to use the exponential image. The exponential image is formed by taking the ratio of a DW image divided by an unweighted image from the same image series and slice position.
"Diffusion weight imaging may be helpful in localizing tumor in patients with previous failed transrectal ultrasound biopsy, with the potential to improve rebiopsy success rates," the Madrid team stated. DWI at 3 tesla combined with T2-weighted imaging had improved sensitivity of 81% to 84%, compared with 54% to 73% for T2-weighted imaging alone. "Sensitivity of ADC values for [prostate cancer] in the peripheral zone is 98%, compared with 81% in the transitional zone although there were no significant differences in specificity," the researchers noted.
Anticancer therapy leads to tumor lysis, loss of cell membrane integrity, increased extracellular space, and thus an increase in ADC values for the tumors. ADC values may be useful as an imaging biomarker for monitoring therapeutic response of prostate cancer to radiotherapy, they wrote.
In assessing the limitations of DWI for detecting prostate cancer, the authors noted that there exist many benign procedures that can decrease ADC values, such as acute prostatitis, benign hyperplasia with dense fibromuscular stroma, or hemorrhage areas that can simulate prostate carcinoma. Another limitation of this sequence includes susceptibility artifacts produced by rectal gas or visceral movement artifacts, and well-defined tumors with glandular predominance present higher ADC values similar to benign prostate tissue, they concluded.
Note: The image on the home page is courtesy of Dr. Jelle Barentsz, PhD.