Coronary CT angiography (CCTA) alone can determine the need for invasive cardiac intervention, according to a multicenter study of more than 15,000 patients presented on Sunday at the European Society of Cardiology meeting in Munich. In patients with high-risk heart disease at CT, revascularization boosted survival, while revascularization had no effect on those considered low risk.
Thus, CCTA results were a strong predictor of the need for intervention in patients with suspected coronary artery disease (CAD), making it a reliable gatekeeper for invasive angiography, principal investigator Dr. James Min, from Cedars-Sinai Medical Center, told AuntMinnie.com in a telephone interview. Over an intermediate-term follow-up, those with high-risk CAD at CCTA were more than twice as likely to die as patients deemed low risk, he said.
Large studies using invasive coronary angiography have already found a survival benefit following intervention -- both percutaneous coronary intervention and surgical coronary revascularization -- in stable patients with high-risk CAD, compared to medical therapy, said Min. But equivalent studies using noninvasive coronary CCTA as a gatekeeper rather than angiography have not been published, he said.
"Some people have said that maybe coronary CT angiographic findings aren't suitable for identifying patients who really should go to the cath lab, and proponents of this sort of thinking have argued for ischemia-guided revascularization," rather than angiographic guidance, he said. "Certainly that's the way we've done it for the past 30 years, and myocardial perfusion imaging by nuclear stress testing has been the dominant force, at least here in the U.S., for evaluating patients with ischemia."
A large-scale study is under way to determine whether ischemia- or angiographically based intervention is superior, he said, but even now there is some evidence that CCTA using fractional flow reserve measurements to guide coronary intervention can predict whether intervention will help certain patients live longer.
The current study, also presented in June at the International Society for Computed Tomography (ISCT) annual meeting and recently submitted for publication, examines the angiographic side, evaluating the utility of CCTA alone for predicting the need for revascularization.
Using a database from the worldwide 32,000-patient Coronary CT Angiography Evaluation for Clinical Outcomes (CONFIRM) study, the researchers sought to determine whether revascularization is associated with improved event-free survival when compared to standard medical therapy alone, Min said. In the study, patients were divided according to high- or low-risk CAD, based on CCTA results.
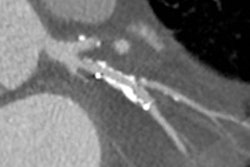
The investigators followed 15,233 patients after CCTA images were acquired on several different 64-detector-row scanners. Images were acquired at 64 x 0.625-mm or 0.750-mm collimation, 100 kV or 120 kV tube voltage, and 400 to 650 effective mA. Images were evaluated by highly experienced cardiologists or radiologists in each center, who visually scored coronary segments using a 16-segment coronary artery model.
All study subjects were referred from eight centers in six countries for cardiac imaging but without known CAD. They were followed for a median of 2.1 years, Min said. Patients were divided according to their risk of coronary disease, with the high-risk category including the following:
- Two-vessel coronary artery disease plus proximal left anterior descending (LAD) artery involvement
- Three-vessel disease
- Left main coronary artery disease
The patients were then further categorized into one of two treatment groups:
- Coronary revascularization (n = 1,103; 2.2% mortality)
- Medical therapy alone (n =14,120, 1.1% mortality)
The study was observational, so to account for the nonrandomized referral for revascularization, Min and colleagues developed a propensity score using logistic regression to identify variables that influenced the decision to refer patients for revascularization -- thereby simulating a randomized trial, Min said. The propensity score model showed that obstructive CAD is the most influential factor for referral, followed by interaction of obstructive CAD with a high pretest likelihood of CAD (p = 0.0344).
 |
| Above, results show survival benefit for revascularization in high-risk patients after CCTA. Below, the benefits of intervention increased with the number of affected vessels. All images courtesy of Dr. James Min. |
 |
The researchers measured the effectiveness of CCTA in determining which patients would benefit from revascularization by calculating hazard ratios (HR) for risk of death among high-risk patients in both the intervention and nonintervention groups. They found a lower risk of death in the intervention group (HR = 0.38, 95% confidence interval [CI]: 0.18-0.83), reflecting a 62% reduction in mortality.
On the other hand, high-risk patients who did not get revascularized experienced a higher death risk (HR = 3.24, 95% CI: 0.76-13.89), but the difference was not statistically significant.
 |
| The number of lives saved with revascularization increased for patients with high-risk disease. |
"If you have high-risk coronary disease, lives are saved [by revascularization], and if you have low-risk coronary disease, no lives are saved," Min said.
Thus, revascularization for high-risk coronary artery disease -- including two-vessel disease with proximal LAD involvement, three-vessel disease, and left main disease -- confers a survival benefit in an intermediate-term follow-up period, according to Min.
"These findings may guide therapeutic decision-making and a referral to invasive angiography in individuals with CTA-identified obstructive coronary artery disease," Min said.
Future studies should examine whether CCTA can improve the appropriateness of referral for cardiac catheterization, he said.