Hysterosalpingography (HSG), a common technique in determining infertility in women, should be more selectively indicated, Swiss researchers found. However, despite its high false-positive rate, it still remains a valuable tool, they noted.
Approximately 15% of couples are affected by infertility, and some of the common causes include ovulation disorders (37%) and tubal damage (18%). The other 45% are problems related to the male partner (Insights into Imaging, 16 July 2012). To assess the problem in women, physicians use HSG specifically to examine uterine wall irregularities, intrauterine adhesions, and congenital abnormalities.
While transvaginal ultrasound is usually the first choice for infertility problems, its usefulness is limited because it cannot assess the morphology and patency of the fallopian tubes -- HSG can. HSG studies have been shown to be important for selecting patients for diagnostic laparoscopy with chromopertubation. Dr. Adrian Schankath from the Institute of Radiology, Kantonsspital Baden, in Baden, Switzerland, and colleagues evaluated all pathologies that were diagnosed by HSG in the workup of female infertility at their institution during a five-year period. They set out to describe the spectrum of diagnostic findings and correlate the diagnostic findings with clinical findings and outcomes.
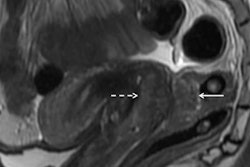
 A 35-year-old patient with an irregular-shaped defect localized at the right side of the cervix, which was identified as a myoma using transvaginal sonography. No tubal pathology. No follow-up information was available for this external patient. All images courtesy of Dr. Adrian Schankath.
A 35-year-old patient with an irregular-shaped defect localized at the right side of the cervix, which was identified as a myoma using transvaginal sonography. No tubal pathology. No follow-up information was available for this external patient. All images courtesy of Dr. Adrian Schankath.Patients were identified by searching the institution's RIS for all HSG exams from September 2006 to April 2010. A total of 411 HSG exams were included in their study, with patients ranging in age from 22 to 42 years.
Of all the HSG exams, 226 (55%) were normal, 94 (23%) showed minor abnormalities, and five (1.2%) were not diagnostic. Eighty-six (21%) examinations were pathological. Twenty-nine patients underwent subsequent laparoscopy -- proximal tubal occlusion diagnosed at HSG was ruled out in nine of 23 cases. Follow-up information was unavailable for 20 patients. Nineteen of 66 patients with follow-up after pathological HSG had at least one subsequent successful pregnancy, while 41 patients had no further treatment and no pregnancies.
 A 32-year-old patient with symmetrically separated uterine cavity (uterus septus). Also, notice venous intravasation of the contrast medium. Laparoscopy and hysteroscopy were performed, and the septum was resected. After this procedure, the patient was lost to follow-up.
A 32-year-old patient with symmetrically separated uterine cavity (uterus septus). Also, notice venous intravasation of the contrast medium. Laparoscopy and hysteroscopy were performed, and the septum was resected. After this procedure, the patient was lost to follow-up.The detection rate for pathologies using HSG was low (21%) and the false-positive rate was high (39%), the researchers concluded.
"This is quite a low detection rate, meaning that we performed four of five HSG procedures in vain," Schankath and colleagues wrote. "This clearly indicates that the indication for HSG at our institution in recent years was too broad."
An alternative could be hysterosalpingo contrast sonography (HyCoSy). It is more demanding for the examiner than HSG, it is better for assessing the uterine cavity than the fallopian tubes, and it has a longer learning curve. However, it also costs less and causes less pain; therefore, no anesthesia is necessary. Plus there is no exposure to radiation.
"Considering that HSG is far more expensive and invasive (i.e., anesthesia, exposure to radiation) than HyCoSy, our aim is to avoid unnecessary HSG exams," they wrote. "Since 2009, we have routinely used CAT [Chlamydia antibody titer] screening to select patients for laparoscopy/hysteroscopy as the first-line exam, and we have set an age limit of 38 years, above which we perform HyCoSy instead of HSG."
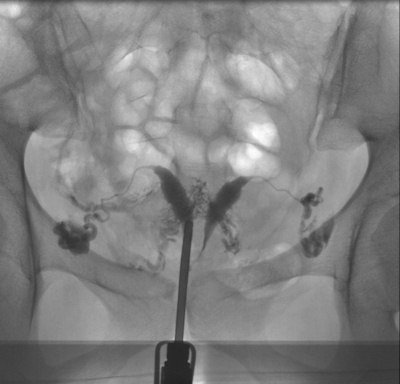
 HSG of a 38-year-old patient with irregular nodular configuration of the right tube (salpingitis isthmica nodosa). The left tube is proximally occluded. Because the patient had decided that she did not want more children, there was no further workup. The HSG was performed to assess the need for anticonception.
HSG of a 38-year-old patient with irregular nodular configuration of the right tube (salpingitis isthmica nodosa). The left tube is proximally occluded. Because the patient had decided that she did not want more children, there was no further workup. The HSG was performed to assess the need for anticonception.The researchers acknowledge the limitations in their study. No follow-up information was available for 23% of the patients with a pathological condition at HSG. It is unknown how many of these patients became pregnant.
"It is likely that patients interrupt their fertility care because of emotional distress and poor prognoses," the authors wrote. "Furthermore, some follow-ups were not available in our study for patients sent to our center only for tubal assessments by their gynecologists or family doctors."
Also, laparoscopic and/or hysteroscopic results were available in only 29 of 411 HSG patients. "This means that there was no information about possibly false-negative exams in the patients with normal HSG exams," they wrote.
From the 86 HSG exams with suspected pathologies, 29 patients had laparoscopy/hysteroscopy, and 20 patients were lost to follow-up, which means it is unknown how many of these patients became pregnant, he added.
Schankath and colleagues don't advise that HSG should be tossed out -- it's a safe, low-cost test and, with the application of propofol sedation, a well-tolerated procedure for tubal assessment. However, it should be performed at the end of the infertility investigation protocol.
"The relatively low percentage (21%) of pathological exams in our population underlines the need for good patient preselection," they wrote. "The high false-positive rate for proximal tubal occlusion (39%), probably due to tubal spasm, demonstrates the importance of antiperistaltic agents and delayed imaging."
There was a high pregnancy rate in patients with pathological HSG -- most were spontaneous without tubal or uterine surgery.
"This could mean that the indication for HSG was too broad or that there could even be a therapeutic effect of the HSG procedure, i.e., improved patency of the fallopian tube because of the flushing during the examination," they wrote.
Because of the study, the workflow at their institution will be adapted. "We will establish HyCoSy as a first-line exam for tubal and uterine factors, and improve the patient selection for primary laparoscopy/hysteroscopy using routine screening for CAT," Schankath and colleagues wrote.