Radiologists must understand the relevant imaging appearances and changes in the revised tumor-node-metastasis (TNM) classification for esophageal cancer's staging system, which is data-driven and better correlates the interplay between the tumor and the node, as well as the histological characteristics of the tumor with the prognosis, according to new research.
The TNM staging system is a vital guide for determining treatment and prognosis in patients with esophageal cancer, but the previous esophageal cancer-stage grouping system was overly simplistic and found not to be consistent with risk adjusted, worldwide data used in the revised TNM staging, noted Dr. Vandan Arora, from the department of clinical radiology at the Christie National Health Service (NHS) Foundation Trust, Manchester, U.K.
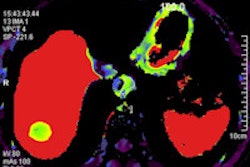
A systematic approach to the interpretation of the staging PET/CT scan enables all clinically relevant features to be adequately assessed and reported, and familiarity with the potential pitfalls and limitations of PET/CT is important to allow a combined multimodality approach for accurate pretreatment staging, he pointed out at the 2012 meeting of the European Society of Gastrointestinal and Abdominal Radiology (ESGAR).
"FDG-PET/CT should be routinely used in all cases for staging of esophageal carcinoma," Arora stated. "FDG-PET/CT is particularly useful in detecting nonregional nodal and occult metastatic disease, thus helping to avoid potentially futile surgery. Multimodality imaging is key for accurate staging, and a dedicated MDT (multidisciplinary team) is essential for optimal management in all (patients)."
Arora and his colleagues sought to highlight the changes in the seventh edition of the TNM staging system for esophageal cancer, outline the clinical utility of PET/CT in staging of esophageal cancer, discuss the pitfalls in staging of esophageal cancer, and illustrate the relative merits and limitations of PET/CT.
For esophageal cancer, surgery offers the best chance of cure, they explained. The poor long-term survival of patients who have complete tumor resection appears to be related to the failure to detect distant metastases at the time of surgery. The survival rates of noncurative surgery are similar to those of nonsurgical therapy using combined chemoradiation. Surgery in patients with advanced disease can be avoided if accurate preoperative staging information is available. Accurate staging in esophageal cancer is therefore essential for guiding therapy, the authors added.
In the American Joint Committee on Cancer staging guidelines (TNM seventh edition), tumor location is simplified, and esophagogastroduodenoscopy is included. T4 is subclassified, regional nodes are redefined, and N classification is done according to number. There are separate age groupings for squamous cell carcinoma and adenocarcinoma, stage groupings are reassigned, and reduced spatial and contrast resolution of PET/CT precludes evaluation of depth of local tumor invasion in most early (T1/2) carcinomas, according to Arora and colleagues.
"The location of primary tumor does not affect prognosis but dictates management, including surgery and radiotherapy planning," he noted. "Depth of tumor invasion is an important criterion for selecting patients for direct surgical resection versus preoperative chemoradiotherapy. PET/CT has limited accuracy for early T staging and endoscopic ultrasound (EUS) is the modality of choice. Certain histological subtypes like low-grade adenocarcinoma are not FDG avid."
PET/CT has a limited role in the assessment of such cases because low-grade uptake in the primary tumor also decreases the sensitivity to detect metastases. False positive inflammatory uptake is often noted after stent insertion, and this activity can make it difficult to differentiate from the uptake in the primary tumor, Arora explained. Evaluation of nonattenuation corrected images may help differentiate true positive versus artifactual uptake, while stenting should be withheld, if possible, prior to the staging with PET/CT.
"Blooming of intense FDG activity in the primary tumor can lead to erroneous overstaging of the primary tumor. Adjusting the intensity of the PET scan, careful reassessment of fat planes between the tumor and adjacent structures, and the angle of contact with the aorta on the corresponding CT images can improve accuracy of T staging," he stated.
Nodal disease is the single most important prognostic factor and remains the epicenter of debate, and FDG uptake within periesophageal lymph nodes that are anatomically close to the primary tumor can make it difficult to differentiate from intense uptake within the esophagus owing to the limited spatial resolution, Arora stressed. EUS has a high sensitivity for detecting metastatic nodes, and is the modality of choice for evaluation of regional periesophageal nodes. He thinks small nodes below the limit of PET/CT resolution are best assessed on EUS.
Detection of metastatic disease at initial evaluation is the most important role of PET/CT in staging of esophageal cancer. Metastatic disease is present in 20% to 30% of patients with esophageal cancer at initial presentation, and distant metastases that are not obvious on anatomic imaging can be seen on PET in up to 5% of cases, estimated Arora. Detection of occult metastatic disease with PET/CT can prevent surgery in patients not suitable for curative resection. The commonest sites of visceral metastases include the lungs, liver, bones, and adrenal glands. Nonregional nodal metastases without involvement of intervening locoregional nodes reportedly occur in 25% of cases.
"Metastases from esophageal cancer can occur in unusual and unexpected locations and may not be detected even on PET/CT," he concluded. "Familiarity with common and unusual sites of disease such as subcutaneous tissues, skeletal muscle, brain, and thyroid gland can improve detection. FDG-PET/CT detected metastases should be confirmed before excluding a patient from surgery, as at least 3.7% are false positives. Unsuspected synchronous neoplasms most commonly in the head and neck, lung, stomach, and colon may be present in 1.5% to 5.5% of patients at presentation."