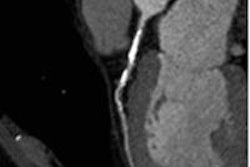
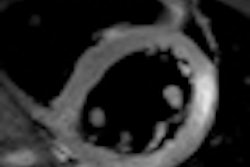
The introduction of 3-tesla MRI into clinical practice has made cardiac MRI a more powerful tool for determining myocardial vitality, perfusion, and function. The technology can help identify coronary stenoses and avoid unnecessary stent implantations in patients with intermediate lesions, researchers from Munich have found.
"The new generation of 3-tesla multitransmit MR systems, with their higher field strength and better spatial resolution, seem to be able to show first pass myocardial perfusion precisely," noted Dr. Ullrich Ebersberger, from the Heart Center Munich-Bogenhausen, affiliated with the University of Munich. "With this new technology prefixed to cardiac catheterization, clinically relevant information can be made accessible."
Earlier this year, Ebersberger and his colleagues began a clinical trial to investigate the ability of MR perfusion imaging at 3-tesla to identify myocardial ischemia, compared with invasive fractional flow reserve (FFR) measurements. They are seeking to recruit 150 patients with an intermediate lesion who underwent cardiac catheterization, including measurement of the myocardial FFR. The exclusion criteria include pregnancy, severe renal dysfunction, instability (e.g., acute myocardial infarction), and contraindications to adenosine, contrast agents, and MRI.
 The annual congress of the European Society of Cardiology (ESC) in Paris attracted a record number of 32,946 participants.
The annual congress of the European Society of Cardiology (ESC) in Paris attracted a record number of 32,946 participants.The Munich group presented their initial findings at the 2011 European Society of Cardiology (ESC) annual congress. Following cardiac catheterization and FFR-measured intermediate lesions, 32 consecutive patients underwent a cardiac MR examination. Three minutes of adenosine infusion occurred, after which perfusion scans (three-slice turbo-field echo, echo-planar imaging) were performed. Rest perfusion was imaged after a 15-minute break, and perfusion images were visually assessed and evaluated on a dedicated workstation by two experienced cardiologists who were unaware of the cardiac catheterization results. Interobserver disagreements were resolved by consensus in a joint session.
MRI was impossible in two of the 32 patients. Of the 90 coronary vessels, eight lesions had an FFR of less than 0.75. The sensitivity and specificity of visual cardiac MR analysis to detect stenoses at a threshold of FFR less than 0.75 were 88% and 99%, respectively.
Coronary artery disease is usually diagnosed by catheterization, and visualization of the coronary arteries is assessed by the examiner, making it prone to a wide spectrum of interobserver differences, especially when it comes to intermediate lesions, Ebersberger explained. Furthermore, the gold standard to assess hemodynamic significance is the measurement of the myocardial FFR, but this method is not in the daily routine and is available only in a fraction of catheter labs worldwide.
"Taking this into account, decision-making, especially in intermediate lesions, remains difficult," he stated. "One major step to simplify the invasive approach concerning intermediate lesions would be to establish a noninvasive procedure that localizes the coronary vessels to intervene ahead of catheterization."