Children who are having difficulty breathing or swallowing, or who are experiencing sepsis or chest pain, are among the most common patients admitted to hospital emergency departments. Radiologists can help clinicians make a rapid diagnosis, start the appropriate treatment, and avoid complications in these nontraumatic thoracic emergency cases.
An article published online 6 July in Insights into Imaging reviews the radiological findings of various pediatric nontraumatic thoracic emergencies, and discusses how clinical presentation influences the choice of radiology exam, with an emphasis of keeping radiation dose as low as possible. X-ray exams remain the primary type of procedure ordered, followed by ultrasound exams and, only when necessary, CT and MRI scans.
The smaller the child, the more urgent need for diagnosis and treatment, according to author Dr. Charlotte de Lange, a pediatric radiologist in the department of diagnostic imaging and intervention at Oslo University Hospital in Norway. Small children may decompensate rapidly with hemodynamic and respiratory failure.
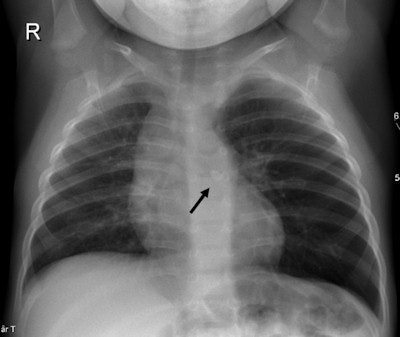 A 1-year-old girl presenting with breathing difficulties after playing with sand. Chest x-ray shows hyperinflation of the left lung and mediastinal shift to the right caused by a check valve mechanism of a small stone (black arrow) visible in the left main bronchus. All images courtesy of Dr. Charlotte de Lange.
A 1-year-old girl presenting with breathing difficulties after playing with sand. Chest x-ray shows hyperinflation of the left lung and mediastinal shift to the right caused by a check valve mechanism of a small stone (black arrow) visible in the left main bronchus. All images courtesy of Dr. Charlotte de Lange.Chest x-rays and ultrasound exams are most commonly performed to diagnose and monitor treatment of newborns and young infants. Respiratory infections, both bacterial and viral, are the most common. Congenital abnormalities of the airways can cause acute respiratory problems during pulmonary infections. While x-rays are initially recommended, multidetector CT scans with multiplanar reconstructions and volume-rendering are superior in depicting the anatomy.
Viral infections are more frequent than bacterial infections in infants and may cause pneumonia. Bacterial infections are more commonly diagnosed in children age 5 and older. Chest x-ray exams are the exam of choice, although approximately 30% of children with viral infections have normal chest radiographs.
Pleural empyema is increasingly being seen, both as a result of improved diagnosis and the reduced number of patients treated with antibiotics, according to de Lange. Chest radiographs and ultrasound exams should be the first exams ordered.

 A 2-week-old baby presenting with increasing breathing difficulties and low oxygen saturation. Left: Chest x-ray shows hyperinflation in the right lung. Right: Chest CT angiography with 3D volume rendering reconstruction reveals a "pulmonary sling" where the aberrant left pulmonary artery arises from the right pulmonary artery and "slings" around the trachea and right main bronchus causing compression and stenoses.
A 2-week-old baby presenting with increasing breathing difficulties and low oxygen saturation. Left: Chest x-ray shows hyperinflation in the right lung. Right: Chest CT angiography with 3D volume rendering reconstruction reveals a "pulmonary sling" where the aberrant left pulmonary artery arises from the right pulmonary artery and "slings" around the trachea and right main bronchus causing compression and stenoses.A CT scan should be ordered only when ultrasound and chest x-ray exams do not distinguish a loculated empyema from an intraparenchymal abscess or a cavitary necrosis/necrotizing pneumonia. Contrast-enhanced CT exams may be required to identify the position of drains, loculations, and parenchymal complications in patients who do not respond to treatment. Exposure to the CT radiation dose may also be warranted when imaging suppurative lung parenchymal complications because of CT's sensitivity and ability to detect and establish the extent of the complication.
X-ray exams should be ordered first for children who have swallowed a foreign object impeding breathing or who have asthma. Radiographs are also recommended for children suspected of having congenital cystic lung disease. However, contrast-enhanced CT is used in patients with persistent symptoms of congenital lobar emphysema to rule out extrinsic vascular compression and to depict the anatomy of the affected lobe and degree of compression.
Vascular rings are congenital anomalies that may be identified with upper gastrointestinal series and echocardiography exams. Cross-sectional imaging with multiplanar and 3D volume rendering reconstructions can help clarify the anatomy. A CT angiography exam may be the scan of choice over MRI because its images show higher spatial resolution of the small caliber vessels and airways, according to de Lange. There also is no need to sedate the patient with this procedure.

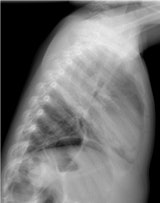 A 4-year-old boy presenting with fever and tachypnea. Left: Chest x-ray antero-posterior view. Right: Lateral view reveals an opacity without volume reduction in the right upper lobe, consistent with lobar pneumonia.
A 4-year-old boy presenting with fever and tachypnea. Left: Chest x-ray antero-posterior view. Right: Lateral view reveals an opacity without volume reduction in the right upper lobe, consistent with lobar pneumonia.Limiting radiation dose exposure to a pediatric patient is of paramount importance, de Lange noted. "When ionizing techniques are considered necessary, dose-reducing equipment and protocols for pediatric examinations are mandatory, following established international guidelines," she wrote. When x-ray exams are performed, automatic exposure control and prefilter exchange should be used, along with the lowest pulse frequency possible and radiation-free adjustment of object positioning.
CT exams of the thorax should always be performed with adjusted imaging parameters for children, with tube voltage at 80-100 kVp. Automatic dose modulation software should be used and also in-place breast shields, as they reduce the radiation to breast tissue and do not affect image quality.
A variety of conditions may cause pediatric thoracic emergencies, which may be life-threatening. "Radiology has become increasingly important in the acute management of these emergencies," de Lange concluded. "A skilled radiologist familiar with pediatric pathological conditions plays an important role in helping clinicians to ascertain the diagnosis and to start adequate treatment."