The forthcoming update to the widely recognized BI-RADS MRI lexicon should help to resolve ambiguity arising from the varied descriptions of enhancement in reports. The update by the American College of Radiology (ACR), due out in November ahead of the RSNA meeting, will use most of the same terminologies found in the original 2003 publication, but a key addition is the relatively new concept of background parenchymal enhancement.
"Background parenchymal enhancement is something that imagers around the world will be happy to report, but will have to get to know," said Dr. Debra Ikeda, professor of radiology and director of the breast imaging section at Stanford University in California, at this month's International Symposium on State-of-the-Art Imaging (iSi 2011) in Bordeaux, France. "It's like reporting breast density on the mammogram. There will be a steep learning curve because right now inexperienced doctors don't know what to do with normal enhancing tissue."
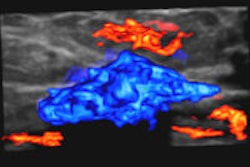
 A certain degree of mild background parenchymal enhancement can be deemed normal due to fluctuating hormone levels, but even moderate enhancement may hide invasive or noninvasive cancer, and radiologists will have to learn to tell the difference, Dr. Debra Ikeda said.
A certain degree of mild background parenchymal enhancement can be deemed normal due to fluctuating hormone levels, but even moderate enhancement may hide invasive or noninvasive cancer, and radiologists will have to learn to tell the difference, Dr. Debra Ikeda said.
With so many U.S. medical professionals facing legal battles for allegedly missing cancer, there is a tendency to "overdescribe" enhancement -- one of the possible signs of malignancy -- and report it as potentially suspicious. However, normal fibroglandular tissue may enhance slightly to reveal a stippled pattern -- i.e., tiny dots of enhancement separated by nonenhancing tissue that may be confluent at times.
Previously, all enhancement was deemed abnormal, but breast parenchyma consists of fibrocystic changes that enhance, which is accentuated by fluctuating hormones. To date, many radiologists have put this newly named background of parenchymal enhancement into the category of BI-RADS 3, when the tissue is actually normal, Ikeda told delegates.
"This is like taking a normal mammogram and saying that the normal tissue visualized is a BI-RADS 3," she noted.
In addition, many different terms, such as "diffuse enhancement" and "regional diffuse stippled enhancement," were used because radiologists didn't know they were looking at normal tissue. Now it is clearer that background parenchymal enhancement is a normal finding and one term will describe it, rather than the many used previously.
"Radiologists the world over will have to learn to distinguish normal enhancing tissue from cancer, but now we have the terms to describe it. Hopefully, the use of BI-RADS 3 should drop," Ikeda said.
BI-RADS 3 should only be used for unique findings above and beyond background. Its descriptors have been adapted from mammography BI-RADS for uniformity. Other changes to BI-RADS classification concern the BI-RADS 0 category to request additional imaging, and which the updated lexicon specifies should only be used to prevent a biopsy.
Besides other changes to morphological mass and nonmass descriptors, the update will also have a new implants section that will describe implant ruptures. Furthermore, it will stipulate the need for combined reporting for optimal ultrasound, MRI, and mammography correlation.
"Reports should not only describe the finding but also how it should be biopsied. For example, with a breast MRI that does not show existing calcifications, the report should state that these be localized with mammography. If lesion enhancement can't be seen by ultrasound, reports should specify that it should be biopsied by MRI," she said.
Ikeda has been director of the Stanford breast imaging section since 1992. Her ongoing research is focusing on diagnosis with MRI and MRI-guided biopsy, as well as new pulse sequence development. Among her new projects are imaging of Asian women, evaluation of breast density, imaging of accelerated partial-breast irradiation, whole-breast ultrasound, and digital mammography with computer-aided detection (CAD). Future projects include optical imaging, and there are plans to incorporate molecular imaging techniques developed at the Clark Center into Stanford's breast cancer research.
In the clinical trial arena, Ikeda is currently recruiting patients for an adjunctive efficacy study of the SoftScan optical breast imaging system, as well as a study of breast density and the role of preoperative mammography, ultrasound, elastography, and MRI. Recruitment is complete for a survey of optical measures of breast tissue in the clinic.
|
|
||||||||||||||||||
|
||
| Source for all tables: ACR BI-RADS Committee. Draft for Breast MRI Lexicon 2nd Edition, Spring 2011. |