SINGAPORE - Combining brain MRI and CT radiomic features improves prognosis prediction for lung cancer patients with brain metastasis, according to research presented May 8 at the International Society of Magnetic Resonance in Medicine (ISMRM) meeting.
A team led by presenter Jyun-Ru Chen, PhD, of National Yang Ming Chiao Tung University in Taipei, Taiwan, found that "imaging characteristics of both primary and secondary (metastatic) tumors are valuable for prognostic prediction in lung cancer with brain metastasis."
The one-year survival rate of lung cancer patients with brain metastasis is 28.2%, Chen noted, although previous research has suggested a survival range from one to 120 months. How metastatic and primary tumors are controlled has been shown to be a prognostic factor for lung cancer patients with brain metastasis, but how best to assess this has remained unclear. That's why creating an overall survival prediction model could help clinicians better manage lung cancer patients with brain metastasis, he said.
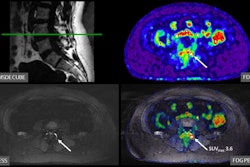
Chen's team explored the efficacy of a lung cancer brain metastasis survival prediction model by combining MRI and CT radiomic imaging features of metastatic and primary tumors. The research included 224 lung cancer patients with brain metastasis from Taipei Veterans General Hospital. All underwent routine MRI that included T1-weighted, contrast-enhanced T1-weighted, and T2-weighted images, as well as contrast-enhanced chest CT imaging.
The group used customized software for image preprocessing and to extract 1,765 brain-metastasis and 593 primary-cancer features from the MRI and contrast-enhanced CT exams. The investigators identified predictors for good prognosis (more than 12 months overall survival) and predictors for poor prognosis (less than 12 months overall survival) and created three models, evaluating their performance using the area under the receiver operating curve (AUROC) measure and assessing for sensitivity, specificity, and accuracy. The three models included one that combined brain metastasis and primary cancer data, another that only included brain metastasis data, and another that included only primary cancer data.
Of the study cohort, 50% had distant metastasis at first imaging, and of these, 45% were brain metastases, the group reported. The study included 101 patients with good prognosis and 123 with poor prognosis.
Overall, the team found that younger age and epidermal growth factor receptor (EGFR) mutation status were associated with a good prognosis among patients with lung cancer brain metastasis.
The model that combined both MRI and CT radiomics features showed the highest AUC (0.79), sensitivity (90%), and accuracy (75%). It also found that the model based on brain-metastasis features (82% of which came from MRI data) performed better than the one based on primary cancer features, Chen reported, noting that the predictors derived from MRIs reflected "strong association between brain-metastasis lesions and prognosis."
"This study [suggests] that survival prediction can be enhanced by combining features of brain metastasis MRI and lung cancer CT," he concluded.