Researchers from Zurich have developed a cumulative clinical risk (CCR) score that may provide an early predictive marker for long-term brain alterations and cognitive impairments in patients with congenital heart disease (CHD). This score may prove valuable in clinical practice to counsel parents about their child's long-term outcome and to aid early identification of those patients at highest risk for long-term brain alterations and provide therapeutic support as early as possible.
"Our findings underscore the clinical relevance of examining cumulative effects of clinical risk and lay a foundation for further, more advanced analyses to improve our prediction of long-term development in children with congenital heart disease," Melanie Ehrler, PhD, a postdoctoral researcher in developmental pediatrics the Child Development Center at Zurich University Children's Hospital, told AuntMinnieEurope.com ahead of her presentation on the topic at the International Society of Magnetic Resonance in Medicine (ISMRM) annual meeting on May 7.
 Melanie Ehrler, PhD.
Melanie Ehrler, PhD.
One surprise for Ehrler is the group did not detect an association between family environmental factors -- such as socioeconomic status, family functioning, and parental mental health -- and brain developmental markers. "Previous research has shown that these family factors are associated with neurodevelopmental/cognitive outcomes, but we could not demonstrate that brain development mediates this effect."
The researchers' CCR score is derived from neonatal, cardiac, and neurological variables, brain connectivity metrics using diffusion MRI, and cognitive outcomes were obtained in 53 CHD adolescents and 75 controls. Patients with CHD who underwent infant open-heart surgery and healthy controls between 10 and 15 years of age were eligible.
Diffusion MRI data were acquired on a GE MR750 MRI scanner (GE HealthCare), with repetition time/echo time (TR/TE) = 7,500/89 ms; matrix = 96x96; field of view (FOV) = 280 mm, slice thickness = 3.6 mm. A total of 35 diffusion-weighted gradient directions were acquired with b = 1,000 s/mm2 and four non-diffusion weighted images. 3D T1-weighted cerebral MRI data were collected with an inversion-recovery prepared, spoiled gradient echo volume (IR-SPGR) with inversion timeTI/TE/TR= 600/5/11 ms and a voxel resolution of 1x1x1mm3.
The researchers built up a CCR score by summing up binary risk factors -- neonatal, cardiac, neurologic -- based on clinically relevant thresholds. Using questionnaires, they assessed family-environmental factors (parental education, parental mental health, and family function). They then acquired cognitive data on executive functioning with a standardized neuropsychological test battery and built an age-adjusted executive function summary score (z-score).
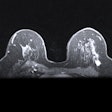
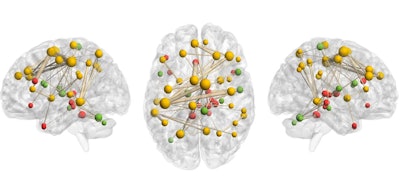 This modeled connectome image shows more cumulative clinical risk correlates strongly with reduced network strength in a fronto-parietal-thalamic network of patients with congenital heart disease. Figure courtesy of Melanie Ehrler, PhD, et al.
This modeled connectome image shows more cumulative clinical risk correlates strongly with reduced network strength in a fronto-parietal-thalamic network of patients with congenital heart disease. Figure courtesy of Melanie Ehrler, PhD, et al.
Higher CCR scores correlated with weaker brain network strength in a fronto-parietal-thalamic network, lower network segregation and poorer cognitive function, independent of family-environmental factors, Ehrler stated. "These findings underscore the need for early risk assessment to predict brain development and aid vulnerable adolescents with CHD."
Clinical implications
The study provides important evidence that structural brain network alterations persist into adolescence, and it shows that patients with CHD, who face a cumulative exposure to multiple clinical risk factors over time, are particularly vulnerable to alterations in structural brain networks and poorer executive functioning. "Quantifying the cumulative load of risk early in life may improve the prediction of long-term brain development of the individual patient. This can help to identify and support the most vulnerable patients as early as possible and to guide clinical and surgical decision-making."
The CCR score is easily applicable in clinical practice, according to Ehrler. "Interestingly, the strength of the associations between the cumulative risk score and MRI markers was quite strong (i.e., moderate to strong effect sizes). This is particularly notable and important because previous research primarily investigated single risk factors and mainly detected small effect sizes."
For follow-up, the group now plans to conduct an additional cerebral MRI and neurodevelopmental evaluation in early adulthood to investigate brain developmental trajectories during a critical period of network formation and white-matter maturation.
The coauthors of this poster are Anna Speckert, Oliver Kretschmar, Ruth Tuura O'Gorman, Beatrice Latal, and Andras Jakab. The team has published a preprint on medrxiv. The study was supported by the Swiss National Science Foundation and the University Research Priority Program's Adaptive Brain Circuits in Development and Learning (AdaBD) of the University of Zurich.