VIENNA - There is no single gold standard for training teams in medicine, but it can pay off to adapt team-working principles from other high-reliability industries such as aviation and Formula 1 motor racing, and integrate them into crisis resource management training, according to emergency room (ER) radiologists.
"Only by continuously evaluating what you do, will we be able to improve our skills and understand the blind spots of our knowledge," said Dr. Vibeke Logager, from the department of diagnostic radiology, Hospital Herlev, University of Copenhagen. "In emergency urogenital imaging, always expect the unexpected."
 Always expect the unexpected in emergency urogenital imaging, according to Dr. Vibeke Logager.
Always expect the unexpected in emergency urogenital imaging, according to Dr. Vibeke Logager.
It is important that the receiving doctors have the relevant clinical information in order to understand whether or not the patient has suffered a high- or low-energy trauma, and therefore the clinical examination and information given in the ER is very important. It is crucial that the team receiving the patient is trained in heavily wounded patients since time is valuable, she noted.
ECR delegates at Monday morning's categorical course will hear speakers discuss how radiologists can prevent misdiagnosis of subtle trauma earlier in the process, and how good follow-up management may contribute to a reduction in morbidity and mortality.
"Imagine a patient with a small subclinical malignant tumor. This patient suffers a mild fall trauma and, due to the pain, is taken to the ER and the primary examination, including analysis of urine, is indicative of not visible hematuria or microscopic hematuria," Logager explained. "Stick to your guidelines/algorithms of patients with hematuria. A patient older than age 40 with microscopic hematuria has the same risk of having a cancer whether there has been an accident or not. If the clinical picture and the image are not the same, then one should always expect the unexpected."
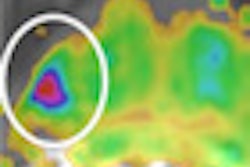
 An 18-year-old female with "after-party amnesia" presented with severe stomach pain and bruises to the head. An investigation showed vaginal bleeding was from the bladder. Full-scale emergency room investigation showed severe left kidney fracture and contusion, but intact vessels and ureter. Three-month follow-up renography shows 28% kidney function on left side as the only sequelae. Image courtesy of Dr. Vibeke Logager.
An 18-year-old female with "after-party amnesia" presented with severe stomach pain and bruises to the head. An investigation showed vaginal bleeding was from the bladder. Full-scale emergency room investigation showed severe left kidney fracture and contusion, but intact vessels and ureter. Three-month follow-up renography shows 28% kidney function on left side as the only sequelae. Image courtesy of Dr. Vibeke Logager.
If the patient is stable, she thinks it is worth doing the full plural phase scans to ensure clinicians have the necessary information to make the right decisions. Radiologists should aim for the maximum imaging if the patient is stable, but if this is not the case, minimize imaging and go straight to the operating room, she recommended.
When dealing with urogenital imaging emergencies, the most important requirement is having specialist knowledge and promoting effective collaboration between clinicians and multidisciplinary teams who are trained in working together. She cautions against complacency; just because experienced radiologists know what to expect and look for in different trauma cases, mistakes can be made, for instance when radiologists find one cause of hematuria (or cause of disease), they tend to stop and think the problem is solved. We should always avoid jumping to conclusions and consider if there are other possibilities, she said.
Close monitoring and early intervention contributes to a reduction in morbidity and mortality in urogenital imaging, according to Dr. Sanjay Agarwal, consultant diagnostic and interventional radiologist at Wrexham Maelor Hospital in Wrexham, U.K. He considers it important to keep the patient's bladder pressure low, noting that high pressure in the bladder is reflected back into the ureter and the kidneys, and is the cause of most problems, especially in cases of infection and deterioration of renal function, leading to kidney damage.
Regarding follow-up of patients with bladder dysfunctions, he advised that there is no agreed follow-up schedule, but, in general, two yearly ultrasound scans and plain x-ray of the kidney, ureter, and bladder should be followed. However, if the patient is symptomatic or the symptoms are not explained by plain radiographs and ultrasound, he cautions that there should be a very low threshold for further imaging.
 Dealing with urogenital emergencies requires dedication, empathy, and focused interest in the subject, points out Dr. Sanjay Agarwal.
Dealing with urogenital emergencies requires dedication, empathy, and focused interest in the subject, points out Dr. Sanjay Agarwal.
"Cross-sectional imaging is not always routinely used at present -- CT due to radiation dose and MRI due to logistics and availability. I am, however, a strong advocate for early and, if necessary, frequent use of these modalities with caution and dose optimization," Agarwal said. "Until a few years ago, use of intravenous urography was routine in several centers, now a CT KUB (unenhanced renal tract CT) can be carried out with lesser dosage and more information. In my opinion, ultralow-dose CT is the way to go, coupled with judicial use of MR urography."
Imaging should be part of good follow-up protocols, which also include clinical consultation and urodynamic assessment, he continued. All these are important to reduce long-term problems with bladder dysfunction, but certain prostheses can make imaging more difficult, such as spinal or other bony metal devices used for fixation of trauma or corrective spinal surgery for deformity. Prostheses associated with the urinary tract that may also cause imaging difficulties are neuromodulation devices, such as sacral nerve stimulators or artificial sphincters.
Agarwal believes that it is especially important to address sexual dysfunction as an integral part of patient management.
"The needs are obviously different between males and females, depending on the cause and extent of physical disability and level of spinal damage. It is not only important to manage the physical and neurological aspects, but also evaluate the psychological and emotional needs," he said.

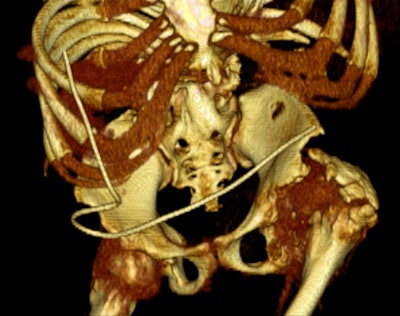 Left: A 33-year-old male with spina bifida. Reconstructed coronal maximum intensity projection CT image shows bilateral staghorn calculi and horse-shoe kidney. Right: A 37-year-old male with spina bifida. 3D reconstruction demonstrates the logistical difficulties with imaging, treatment, and management due to gross bony deformities. Images courtesy of Dr. Sanjay Agarwal.
Left: A 33-year-old male with spina bifida. Reconstructed coronal maximum intensity projection CT image shows bilateral staghorn calculi and horse-shoe kidney. Right: A 37-year-old male with spina bifida. 3D reconstruction demonstrates the logistical difficulties with imaging, treatment, and management due to gross bony deformities. Images courtesy of Dr. Sanjay Agarwal.Currently, there is ongoing research for management of neurogenic bladder dysfunction. In the short term, simple things such as safer tube drainage using biofilm blocking and dispersive agents and closed tube drainage systems may help with reducing infection rates. More complex research is being conducted from multiple angles -- for example, application of gene therapy (use of herpes simplex virus-derived vectors, etc.), development of newer medication (afferent pathway drugs) and tissue regeneration (tissue-engineered autologous augmentation cystoplasty). All will have roles to play in future management of these patients, making this a very exciting time, Agarwal pointed out.
Like Logager, Agarwal believes imaging evaluation is a relatively easy task in this group of patients; more important, you need a multidisciplinary approach to patient management with a full understanding of the pathophysiology and clinical implications, he said. To deal with these patients requires dedication, empathy, and focused interest in the subject. Very promising research is being done in this area, and it will improve long-term outcomes and further reduce morbidity and mortality, he concluded.
Originally published in ECR Today on 11 March 2013.
Copyright © 2013 European Society of Radiology