VIENNA - The delicate balance of power and complex set of interactions between radiologists, patients, and clinicians was the subject of some lively and frank discussion at Sunday's professional challenges session, which followed a novel and original format. Nobody held back, considered opinions were given, and niggling issues were teased out by the panel members, audience, and the one brave clinician in the packed room.
Among the panel members were two radiologists, a medical ethicist, and a clinician. Former ECR President Dr. Andy Adam kick-started the session by pointing out that 50% of patients do not realize that radiologists are actually medical doctors.
"I think it's the fault of radiologists because, in many cases, they don't always deal with patients like a doctor typically does. Radiologists abandon patients and damage themselves as a profession, disadvantage patients, and increase healthcare costs," asserted Adam, a professor of interventional radiology at the University of London and clinical director of imaging and medical physics at King's College, U.K. "Getting closer to the patient will make radiologists more relevant. In many situations, they should impart appropriate information and behave like a real doctor."
 Moderator Wofgang Wagner, Chairman Claus D. Claussen, Jim Reekers, Markus Peck-Radosavljevic, Andy Adam, and Georg Marckmann. Image courtesy of the European Society of Radiology.
Moderator Wofgang Wagner, Chairman Claus D. Claussen, Jim Reekers, Markus Peck-Radosavljevic, Andy Adam, and Georg Marckmann. Image courtesy of the European Society of Radiology.The token clinician, Dr. Markus Peck-Radosavljevic, an associate professor of medicine at the department of gastroenterology and hepatology at Vienna Medical University, said he felt it was important that radiologists spoke to him directly with the details.
"It's more a matter of practicality, resources, and time. But if I have to decide between the radiologist speaking to the patient so I get the report in two weeks, versus the radiologist not speaking to the patient and I get results in two days, then I prefer the latter," he said.
Medical ethicist Dr. Georg Marckmann, from Ludwig Maximilian University of Munich offered his thoughts by saying radiologists were physicians and therefore had the same professional obligations as any physician to patients, including respecting their well-being, using the best available diagnostic and therapeutic interventions, and minimising harm, respecting patient autonomy, and contributing to social justice.
"Healthcare delivery has evolved to a complex system of care where different disciplines and professionals work together. It is like a rather complex orchestra, but the interesting question is who is in the orchestra and who plays first violin?" he commented.
Dr. Jim Reekers, an interventional radiologist at the University of Amsterdam, illustrated his point by describing a scenario in which an internal medicine clinician either calls a surgeon to come to look at a patient and discuss what to do, or he orders an image from the radiologist. "You don't ask the radiologist to come over and give advice on which image is most appropriate. With a surgeon you have respect, but with a radiologist you order him to do an image. That's the difference in attitude and where communication has gone wrong."
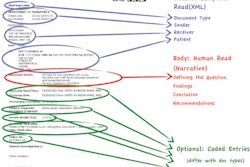
Moving on to the radiologist-patient relationship, Adam said that done properly, radiologist-patient communication can work to the patient's advantage clinically but also benefit the hospital's finances. He described a typical patient pathway in a U.K. hospital with requests, reports, and scans moving between general practitioners, clinicians, radiologists, and multidisciplinary meetings, and eventually reaching a surgeon.
"This could potentially take weeks," he said. "This is a crazy way to practice medicine in the 21st century. There's no earthly reason why the radiologist can't interact with the referring clinician and the patient early on, and organize investigations like a proper doctor."
"This would not only save money but adrenaline, anxiety, and worry for the patients and their families," Adam argued. "I reinforce my point that a radiologist is a doctor, and he or she has to work like a doctor and communicate with the patient appropriately."
Audience members were invited to participate and did so with enthusiasm. There was controversy about the language used to "order" or "request" an examination from a radiologist, with one U.S.-based surgeon saying that there were too many technologies and that their availability needed to be reined in.
"It's like ordering from a menu of exams," the delegate remarked.
An Irish radiologist waded in, disagreeing with the idea that radiologists receive "orders," saying that he only got "requests" and that if he felt it was inappropriate to perform the request, he would deny it. On the clinician-radiologist relationship, he said, "I have a close relationship with the clinician, I advise on the best tests, I get back to them on the next steps." So addressing the panel, he said that he thought their points of view were extreme. "If you need to communicate with your clinician, then just pick up the phone." The panel's one clinician agreed with him.
A radiologist from Australia piped up to make her point that she believed radiologists were there to interact with the patients. "I think we should always talk to them first. We need to think, 'If it was me having the scan done, what would I want.' We need to put ourselves in their shoes," she said.
"I always tell my patients that this information is part of a jigsaw puzzle, and the other bits of the puzzle are in the hands of the referring doctor, and if they go back to the doctor, they will find the rest of the jigsaw is put together," she said.
This innovative session was never going to lead to universal agreement, but it certainly helped to raise and address important issues facing the profession.
Originally published in ECR Today on 11 March 2013.
Copyright © 2013 European Society of Radiology