VIENNA - Imaging has helped to improve heart disease treatment and prevention. Today, diagnosing cardiac patients has become routine for many radiologists. However, some may not know of recent developments in this field. A panel of experts will update both general and specialized radiologists with the latest information available on cardiac imaging, during the dedicated Mini Course "Organs from A to Z: Heart," which starts today.
After an introduction to heart anatomy and the main imaging protocols, the course will focus on valvular diseases and cardiomyopathies, two pathologies commonly encountered in radiology practices. "Anyone who has MRI equipment and has experience of cardiac cases is likely to be asked by a cardiologist to diagnose one of these patients someday," said Dr. Konstantin Nikolaou, a professor of radiology and vice chair of the department of clinical radiology at Munich University Hospital in Germany.
MRI allows radiologists to assess cardiomyopathies and valvular disease with a very high level of precision, even though echocardiography -- especially in skilled hands -- often proves sufficient. "MRI is very good at quantifying the degree of a cardiac valve problem. By using MRI, you can determine the direction and quantity of blood flow, and thereby assess a valvular insufficiency or stenosis with great accuracy," explained Nikolaou, who will chair the Mini Course.
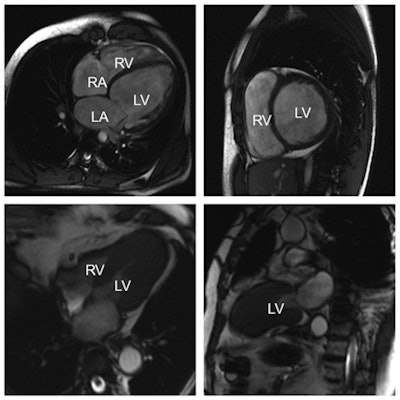 Top row: Example of a dilated cardiomyopathy (DCM). Cine-MR images in four-chamber view (left) and short-axis view (right) at end-diastole show significant dilatation of the left ventricular cavity. Ejection fraction was less than 35% in this patient. (RA = right atrium; LA = left atrium; RV = right ventricle; LV = left ventricle). Bottom row: Example of an asymmetrical, apical hypertrophic cardiomyopathy (HCM). Cine-MR images in a four-chamber (left) and two-chamber view (right) in systole show a markedly thickened left ventricular myocardium predominantly of the apex, as compared with the basal segments. All images courtesy of Dr. Konstantin Nikolaou.
Top row: Example of a dilated cardiomyopathy (DCM). Cine-MR images in four-chamber view (left) and short-axis view (right) at end-diastole show significant dilatation of the left ventricular cavity. Ejection fraction was less than 35% in this patient. (RA = right atrium; LA = left atrium; RV = right ventricle; LV = left ventricle). Bottom row: Example of an asymmetrical, apical hypertrophic cardiomyopathy (HCM). Cine-MR images in a four-chamber (left) and two-chamber view (right) in systole show a markedly thickened left ventricular myocardium predominantly of the apex, as compared with the basal segments. All images courtesy of Dr. Konstantin Nikolaou.MRI can also be crucial in diagnosing congenital heart diseases, in cases in which ultrasound proves inconclusive. But the problem with MRI in cardiac imaging remains its availability; often limited to universities or dedicated centers, and often with long waiting lists. Congenital diseases are usually assessed in babies or very young children, for whom it is almost impossible to lie still for an MRI for 45 minutes without sedation or general anesthesia, which can present a risk for children. Consequently, radiologists may choose to use CT in younger patients, as it offers rapid diagnosis and has become safer in recent years, with a significant improvement in dose reduction strategies.
"We perform more and more CT examinations to assess congenital heart disease in both adults and younger patients, even newborns, because new acquisition techniques use a lower radiation dose. CT gives you a very fast diagnosis. Sometimes you can't or don't want to sedate a little child for 45 minutes for an MRI exam. The patient may also be too sick to lie still for so long. CT has thus become an alternative, even if MRI remains the first option," Nikolaou pointed out.
The third part of the session will focus on ischemic heart disease, the main cause of death in Western countries, before cancer. Catheter angiographies performed by cardiologists remain an excellent way to assess the risk of developing a cardiac event, but it is an invasive procedure with risks.
Here as well, CT presents a number of advantages. It has been used for more than 20 years to provide noninvasive examinations of the coronary arteries. Traditionally, CT's two main applications in cardiac imaging are calcium screening, which measures the amount of calcium in the arteries, and coronary CT angiography, which can reveal the degree of stenosis of the vessels.
CT angiography actually goes beyond risk assessment, and is typically carried out in a symptomatic patient with suspected coronary artery disease to exclude stenosis, for instance in a patient presenting with chest pain but not a typical angina. In such cases, the radiologist might be asked to perform a coronary CT angiography to prove or exclude the existence of stenosis and further characterize potential disease of the coronary arteries.
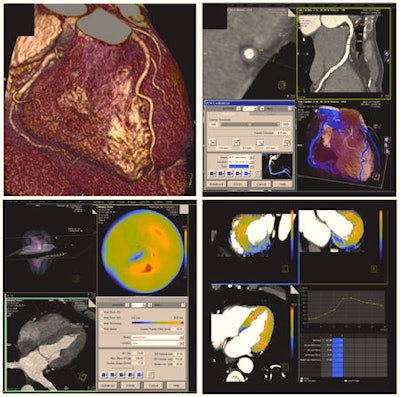 Today, contrast-enhanced cardiac CT is mainly used to display cardiac and coronary morphology in motionless images. Results can be displayed through volume-rendering techniques (top left) or dedicated software can be used for a detailed analysis of the coronary arteries and potential coronary artery stenosis -- e.g., using curved multiplanar reformats (top right). However, cardiac CT can also analyze cardiac function (global functional parameters and also regional wall motion, displayed in color maps, bottom left). Recent developments and research are focusing on the assessment of myocardial perfusion -- e.g., using dynamic, time-resolved acquisition modes. This way, blood flow through the myocardium can be displayed in color maps or in time-density curves, potentially allowing assessment of the hemodynamic significance of a given coronary artery stenosis (bottom right).
Today, contrast-enhanced cardiac CT is mainly used to display cardiac and coronary morphology in motionless images. Results can be displayed through volume-rendering techniques (top left) or dedicated software can be used for a detailed analysis of the coronary arteries and potential coronary artery stenosis -- e.g., using curved multiplanar reformats (top right). However, cardiac CT can also analyze cardiac function (global functional parameters and also regional wall motion, displayed in color maps, bottom left). Recent developments and research are focusing on the assessment of myocardial perfusion -- e.g., using dynamic, time-resolved acquisition modes. This way, blood flow through the myocardium can be displayed in color maps or in time-density curves, potentially allowing assessment of the hemodynamic significance of a given coronary artery stenosis (bottom right).In addition, researchers have started to use CT to differentiate between types of coronary plaques. Plaques in the vessel wall not only consist of calcium, but also other tissues such as fibrotic, fibro-fatty and necrotic core tissues, all of which may have a predictive value for the patient. "Today, we would hardly make a clinical decision based on CT plaque imaging alone, but it is one of the important topics in cardiac CT research," Nikolaou said.
Current scientific studies have also been focusing on a more detailed analysis of the myocardium -- i.e., applying CT techniques instead of MRI to depict myocardial perfusion defects -- in order to gain time in the diagnostic process. "Patients are sometimes referred to nuclear medicine, or for an MRI scan for perfusion tests, when CT angiography results are inconclusive. We now try to get information on perfusion during the CT examination, by adding a CT perfusion scan to angiography," he said. "This would potentially enable us to get the whole picture in one examination and make a better clinical decision, based on the functional relevance of a given stenosis. Whether these rather new CT techniques will be used in everyday clinical routine is still not clear," he added.
Study results indicate that researchers will probably soon be able to find the perfusion defect caused by a stenosis with CT, the radiologist believes. "Depending on correct patient selection in accordance with cardiology, I think that we will, in a few years, start to use CT perfusion or CT dual imaging of the myocardium for the assessment of functional relevance of a coronary artery stenosis detected in CT angiography," he said.
MRI and nuclear medicine tests still set the standard for assessing myocardium in ischemic heart disease, as both of these imaging modalities can provide very detailed information on the ischemic myocardium. For instance, in a patient with suspected ischemic heart disease, MRI can reveal typical lesions in the myocardium caused by an infarct.
MRI is also able to help establish whether a myocardial infarction happened recently or a few years ago. "If you use water-weighted images, the presence of edema in the myocardium means that this is a recent infarct," Nikolaou said.
MRI is the first modality in more complex or known cases of coronary artery or ischemic heart disease, for instance if a patient received bypass surgery, suffered known infarcts, or underwent coronary interventions (e.g., with stent implantation). "CT is good for assessing ischemic heart disease at an early stage or for a first diagnosis, but MRI does a better job if it is a more complex case. It gives information on the perfusion defect, old events, if the stent is still patent, etc." he concluded.
Mini Course:
Organs from A to Z: Heart
Thursday, 7 March, 16:00-17:30, Room L/M
MC 322: Technical and anatomical fundamentals for imaging the heart
Moderator: A. de Roos; Leiden/NL
- Anatomy: too many details in cardiac imaging?
A.J.B.S Madureira; Porto/PT - Examination protocols for imaging the heart: CT
H. Alkadhi; Zurich/CH - Examination protocols for imaging the heart: MRI
N.L. Kelekis; Athens/GR
A. de Roos; Leiden/NL
Friday, 8 March, 08:30-10:00, Room L/M
MC 422: Non-ischaemic heart disease
Moderator: V.E. Sinitsyn; Moscow/RU
- Congenital heart disease
M. Gutberlet; Leipzig/DE - Valvular disease
J. Bogaert; Leuven/BE - Cardiomyopathies
P. Sipola; Kuopio/FI
V.E. Sinitsyn; Moscow/RU
Friday, 8 March, 16:00-17:30, Room L/M
MC 722: Ischaemic heart disease
Moderator: C. Catalano; Rome/IT
- Imaging of the coronary arteries: the Holy Grail
G. Roditi; Glasgow/UK - The ischaemic myocardium: what to do?
C. Loewe; Vienna/AT - The ischaemic heart after treatment: still alive?
G. Bastarrika; Pamplona/ES
C. Catalano; Rome/IT
Originally published in ECR Today on 7 March 2013.
Copyright © 2013 European Society of Radiology