VIENNA - Winston Churchill, the former British Prime Minister, smoked heavily and was overweight, yet he lived to the age of 90. Others live healthily and die well before they reach 60. Emerging techniques for diagnosing atherosclerosis promise to explain why this apparent contradiction occurs and make medicine much more patient-specific.
"Now large-scale studies using predictive markers in low-, moderate-, and high-risk patients must show which are best and most cost-effective for assessing atherosclerotic risk," said Dr. Tobias Saam, attending clinical radiologist at Downtown Campus of the Ludwig Maximilian University in Munich, pointing to a German study currently in the planning stage that will involve tens of thousands of patients using advanced MR techniques for cardiovascular imaging to identify optimal imaging and biomarkers.
Atherosclerosis is a chronic disease of the vessel wall, accounting for more than a quarter of ischemic strokes and the majority of myocardial infarctions and cardiac sudden deaths. New methods to image the vessel wall can help radiologists understand the pathophysiology of the disease and identify what makes for increased cardio- or cerebrovascular risk, moving away from the old concept of only looking at luminal stenosis that often indicated end-stage disease.
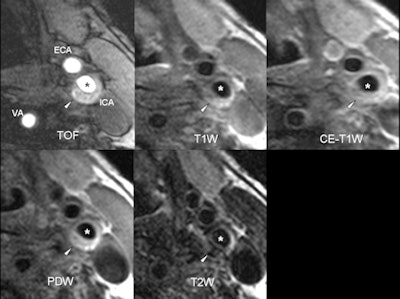 |
| Axial MR images of an 82-year-old symptomatic patient without cardiovascular risk factors. The patient suffered a stroke ipsilateral to the left carotid artery five days before the MRI examination. The arrowhead points to a complicated eccentric plaque that is hyperintense on time-of-flight (TOF) and T1-weighted images, indicative of intraplaque hemorrhage. Of note, no luminal stenosis in the ICA (asterisk) can be seen. The images illustrate that cerebrovascular events due to macroangiopathic carotid disease can occur in the absence of luminal stenosis. ICA = internal carotid artery, ECA = external carotid artery, VA = vertebral artery, PDW = proton density-weighted image. (Provided by Dr. Tobias Saam) |
"Vessel wall imaging is an exciting field which has entered clinical practice, and its role will grow. Luminal stenosis alone is insufficient to predict plaque vulnerability," said Prof. Maximilian Reiser, director of clinical radiology at Ludwig Maximilian University, former European Congress of Radiology (ECR) and European Society of Radiology (ESR) president, and chair of today's New Horizons session. "It is mandatory for radiologists to know more about new opportunities which will be increasingly used in practice."
These techniques can also provide a snapshot at various time points to monitor drugs and intervention and demonstrate disease progression and regression.
"If methods are optimized, we may be able to decide which patients harbor high-risk atherosclerotic plaques that will ultimately cause myocardial infarction or stroke, which will significantly impact patient management," he noted.
Specifically, advanced techniques such as black-blood MRI, intravascular ultrasound (IVUS), and PET/CT are helping to identify risk by providing detailed information on plaque composition, morphology, and activity in patients with atherosclerosis. In addition, because atherosclerosis is a chronic disease that starts in a person's 20s and 30s and develops over decades, with plaque burden increasing by around 2% per year, drugs to decrease plaque load by as much as 10% could be very effective.
"Drugs to slow disease progression could have a huge impact on a patient's outcome. Data suggests certain drugs may halt progression altogether. In addition, some exciting new preliminary results will be discussed as to whether the disease is reversible with certain treatment," said Saam, who will be speaking at today's session about how reversible atherosclerosis currently appears.
 |
| Images show coronary CT angiograms of three different patients of similar age and with similar risk factor profiles. Images were acquired with a dual-source CT system (Siemens Flash; radiation dose <1.5 mSv for each patient). Patient 1 has normal coronary arteries. Patient 2 has a significant coronary stenosis in the absence of coronary calcifications (arrow). Patient 3 has a large soft plaque (arrowheads) and smaller calcified plaques in the absence of luminal narrowing. According to a recent meta-analysis by Bamberg et al, patients 2 and 3 have an increased risk of future cardiovascular events compared to patient 1, despite similarities of age and risk factor profile. Hazard ratio for patient 2 = 10.7; hazard ratio for patient 3 = 4.5. (Provided by Dr. Fabian Bamberg) |
Lowered radiation dose means that CT angiography (CTA) has become far more acceptable in intermediate-risk patients for assessing the future risk of a major cardiac event, such as myocardial infarction or the need of coronary stenting. CTA used to involve a dose of 10 to 20 mSv, but with the latest scanners, half of patients examined receive less than 1 mSv. Even scanners released in the past five years usually involve a dose of only 3 to 8 mSv. In addition, a recent meta-analysis has shown that the presence of ≥ 1 significant coronary stenosis was associated with an annualized event rate of 11.9%, with a corresponding hazard ratio of 10.74, demonstrating that coronary CTA can be used to identify patients at risk for cardiovascular events.
"Blooming artifacts due to extensive coronary calcifications may hide the extent of stenosis, but this can at least in part be compensated for with thinner slices and faster rotation," Reiser said.
The predictive value of PET/CT for events is as yet unclear, although ongoing studies in North America may yield results soon. However, it is clear that PET/CT provides information about inflammation in different vascular territories, which is important for establishing the future risk of plaque rupture. Complementing the section on nuclear medicine, Prof. Michael Schäfers, radiologist at the Centre of Nuclear Medicine, Münster, Germany, will be talking about the role of molecular imaging of atherosclerosis in future clinical practice.
Meanwhile, other techniques are emerging with capacity to predictively identify risk. High-resolution black-blood MRI shows plaque composition and morphology in the carotid arteries in unprecedented detail. IVUS is an effective technique for determining plaque burden in the coronary arteries, and studies suggest that it can be useful to identify the so-called thin-cap fibrous atheroma, a risky lesion in which the thinner the layer of fibrous tissue covering the lipid/necrotic core, the more prone to rupture and the greater the risk of stroke or infarction. More details about these techniques will be heard in the talk by Prof. Jonathan Gillard, professor of neuroradiology at the University of Cambridge, U.K., who will be discussing noninvasive imaging of the vulnerable atherosclerotic plaque.
One of the main problems with vessel wall techniques is that often the only imaging criteria employed to indicate an intervention is the degree of stenosis, regardless of plaque composition. Biological processes such as positive remodeling mean that risky plaques without stenosis may still result in cardiac or cerebral events. In fact, of the ischemic strokes due to atherosclerotic disease, only 10% are watershed infarcts with a high degree of carotid stenosis, whereas 90% of ischemic strokes are caused by thrombosis and distal embolization due to plaque rupture.
"The higher the stenosis, the more likely the existence of a complicated plaque," Saam explained. "However, studies have shown that the majority of myocardial infarctions occur in vessels with less than 50% stenosis. Little is known of the prevalence and the impact of complicated plaques in acute stroke patients without carotid stenosis."
Munich's carotid plaque imaging study (CAPIAS, Carotid Plaque Imaging in Acute Stroke) is using black-blood MRI and conventional ultrasound. It started in February 2011 and is due to end in 2014. It aims to evaluate the prevalence of complicated plaques in nonobstructive carotid disease and to evaluate whether patients with a complicated plaque at baseline have a higher risk of recurrent stroke. Depending on the results, this study may have implications for diagnostic decision-making and provide the basis for the planning of targeted interventional studies.
Another research area is the identification of imaging-based plaque factors that accelerate atherosclerotic disease process and/or can identify patients at increased risk of cardiovascular events. Some of these markers, such as coronary calcium scoring by CT, are increasingly used in clinical practice. Using this technique, risk stratification can be substantially improved compared to risk stratification using conventional risk factors alone. Also, MRI-based detection of intraplaque hemorrhage, an indicator of plaque instability, has been identified as being of great potential use. Studies suggest that hemorrhage accelerates atherosclerotic disease process.
The panel discussion on predictive markers is likely to be lively, as delegates and speakers discuss the multitude of different markers for use with the various modalities.
Originally published in ECR Today March 4, 2012.
Copyright © 2012 European Society of Radiology