Coronary plaque rupture and thin-cap fibroatheroma are common in patients with coronary artery disease, for whom clinical factors and bad habits like smoking increase the risk even more, according to an Italian meta-analysis in the European Heart Journal -- Cardiovascular Imaging.
The study surveyed the prevalence and clinical predictors of coronary plaque rupture in more than 150 patients with coronary artery disease. It examined so-called "culprit lesions" in patients who had coronary plaque rupture or thin-cap fibroatheroma at optical coherence tomography (OCT) after coronary CT angiography.
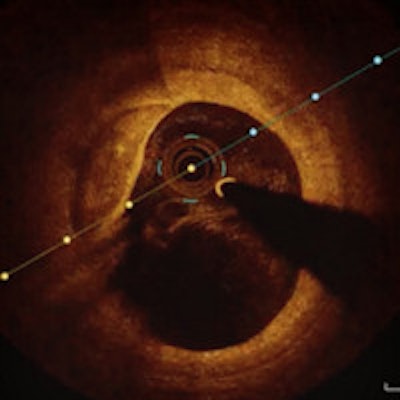
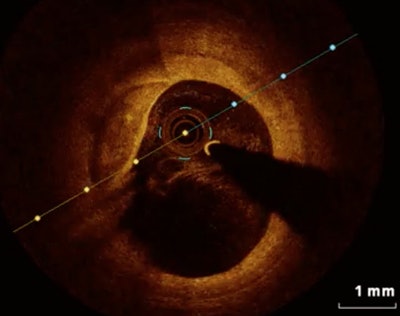 Thin-cap fibroatheroma at optical coherence tomography. Image courtesy of Dr. Mario Iannaccone.
Thin-cap fibroatheroma at optical coherence tomography. Image courtesy of Dr. Mario Iannaccone.The prevalence of both coronary plaque rupture and thin-cap fibroatheroma was high, at more than 48% of this population for both manifestations, the authors reported. Thin-cap fibroatheroma seems to be a strong predictor of coronary plaque rupture in all acute coronary syndrome scenarios, they wrote (European Heart Journal -- Cardiovascular Imaging, 27 October 2015).
High rates of coronary plaque rupture and thin-cap fibroatheroma were detected by OCT in all patients with coronary artery disease, especially those with acute coronary syndromes, But the rate was non-negligible even in those with stable coronary disease, wrote Dr. Mario Iannaccone from Citta` della Salute e della Scienza in Turin, Italy, and colleagues at Harvard Medical School in Cambridge, Massachusetts, U.S., and other centers in Asia and Europe.
The results leave intriguing questions in their wake regarding potential trigger events for rupture, Iannaccone told AuntMinnieEurope.com. He also believes that fibroatheroma is a key area for research as a predictor of plaque rupture.
OCT: A better modality
OCT has emerged in recent years as the most accurate modality for intracoronary evaluation, the authors wrote. It does an excellent job in characterization of plaque and is more accurate than intravascular ultrasound.
Nevertheless, the spectrum of presentation for plaque evaluated with OCT varies widely, and "different data have been reported about the incidence of plaque rupture evaluated with OCT," the authors wrote. Thus, the clinical predictors of plaque rupture remain to be defined.
For physicians and interventional cardiologists evaluating these patients, the incidence and predictors of coronary plaque rupture might offer more evaluation of the cardiovascular risk, Iannaccone and colleagues wrote. The study sought to evaluate the prevalence and clinical predictors of coronary plaque rupture at OCT.
Clinical context critical
The pathophysiology of acute coronary syndrome differs substantially from that of stable angina, mostly due to plaque features, the authors explained. Most "culprit lesions" that trigger an acute ischemic event actually turn out to be only moderately stenotic plaques.
"However, when evaluated at autopsy or with intracoronary imaging, they often show a pro-thrombotic pattern with thin-cap fibroatheroma, soft plaques, and thrombus prone to rupture," the authors noted.
The prevalence of culprit plaque rupture is quite variable depending on the clinical context. In postmortem studies, coronary plaque rupture has been found to occur more frequently in patients with sudden cardiac death than acute myocardial infarction.
The meta-analysis included 23 full-text studies, and the prevalence of culprit plaque rupture in thin-cap fibroatheroma was the study's primary endpoints. The study team assessed factors associated with these two findings in a subset of patients with different clinical findings, including ST-elevation myocardial infarction (STEMI) versus non-ST-elevation myocardial infarction (NSTEMI) versus unstable angina.
In their study, Iannaccone and colleagues examined the impact of clinical features on plaque rupture using meta-regression analysis, both in the overall population and in different patient subsets. The prevalence of coronary plaque rupture was 48.1%, while that of thin-cap fibroatheroma was 48.7% at OCT.
STEMI patients fare worse
Patients with STEMI had higher prevalences of both plaque rupture (70.4%) and thin-cap fibroatheroma (76.6%) than NSTEMI patients, with a plaque rupture prevalence of 55.6% and of thin-cap fibroatheroma at 56.3%.
At meta-regression analysis, the only significant predictors of plaque rupture were current smoking (p < 0.001) and the presence of thin-cap fibroatheroma (p = 0.002).
The factors for plaque rupture were different depending on the patient's presentation. The only clinical predictor for STEMI was hypertension (p = 0.001), but NSTEMI and unstable angina had several predictors including diabetes mellitus (p = 0.012) and hyperlipidemia (p = 0.005).
Rates of thin-cap fibroatheroma and plaque rupture were higher in patients with acute coronary syndromes -- especially those hospitalized for STEMI and NSTEMI.
In all acute coronary syndrome scenarios, thin-cap fibroatheroma seems to be a strong predictor of plaque rupture, Iannaccone et al wrote. Finally, they said, most traditional cardiovascular risk factors are predictive of plaque rupture, especially in NSTEMI and unstable angina patients compared with STEMI patients.
As for limitations, the study was observational and not a patient-level analysis, they wrote. Therefore the use of meta-regression analysis must be viewed as a hypothesis, and not as solid evidence of causal associations.
As an imaging modality, OCT is feasible and safe, showing all of the various microstructures of atherosclerotic plaque, they wrote. But why some plaque ruptures lead to a specific acute coronary syndrome such as STEMI or NSTEMI remains unclear, the study team added.
"Certainly, not only plaque rupture, but also other mechanisms such as plaque erosion and calcified nodules contribute to thrombosis, and, associated with various combinations of systemic factors (e.g., hypercoagulability, activation of sympathetic nervous system, increased systemic inflammation) are responsible for different clinical presentations," the authors wrote.
As previous studies have shown, the non-negligible prevalence (6.2%) of plaque rupture in patients with stable coronary artery disease shows the complex relationship between plaque rupture and coronary disease. The absence of such presentations is a key to milder clinical presentations.
There is a high prevalence of coronary plaque rupture and thin-cap fibroatheroma detected by optical coherence tomography in patients with coronary artery disease, especially those with acute coronary syndromes, the authors concluded. Thin-cap fibroatheroma seems to be a strong predictor of coronary plaque rupture in all acute coronary syndromes.
"To me the most interesting point in our paper is that ... while cardiovascular risk factors correlate with plaque rupture in NSTEMI/unstable angina patients, this is not valid for STEMI patients," Iannaccone pointed out in an email to AuntMinnieEurope.com. "This leaves many unanswered hypotheses about the possible trigger event in this subset of patients: Could adrenergic stress be a trigger? Bacterial infection? Inflammation?"
The second point is that thin-cap fibroatheroma could be an interesting method to predict plaque rupture, though it remains to be validated, he wrote. Further study is needed to evaluate if performing preventive coronary stenting based on anatomical criteria of plaque instability could reduce major adverse cardiac events.