VIENNA - Management and treatment of pancreatic cancer patients is a complex and challenging task requiring a multilateral effort across medical specialties. Speakers at today's multidisciplinary session intend to illustrate to European Congress of Radiology (ECR) delegates a unified approach to pancreatic cancer that enables the goals of each specialty to be achieved for timely diagnosis and effective treatment.
With pancreatic cancer, surgeons need to know if there are any liver metastases because they will usually prevent surgical treatment. Percutaneous biopsies of pancreatic cancer have an inaccuracy rate of up to 25%, so diagnostic imaging plays a central role. The detection of metastases depends on size, histology, and the reaction of contrast agents, and to a lesser extent on the technique, when detecting metastases larger than 2 cm. Accuracy is lower where metastases smaller than 2 cm in size are concerned. Therefore depicting small liver metastases by means of diagnostic imaging before and after contrast administration may avoid unnecessary laparotomies, which are always associated with a different level of morbidity and mortality.
At this afternoon's session, attendees will learn about which pathological criteria are necessary to diagnose liver metastases and the importance of histological subtyping such as adenocarcinoma versus endocrine neoplasm. They will also they find out about the sensitivity of different imaging modalities in detecting liver metastases and the improvement in sensitivity after the administration of liver-specific contrast agents, as well as the imaging criteria for the differential diagnosis of focal liver lesions. The issue of positive lymph node presence will be addressed too.
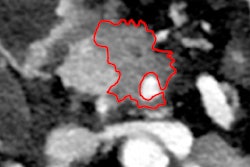
 Axial contrast-enhanced CT scan during the pancreatic phase of the dynamic study shows a hypodense lesion in the head of the pancreas (arrow), representing a small adenocarcinoma at surgico-pathological examination. All images courtesy of Dr. Riccardo Manfredi.
Axial contrast-enhanced CT scan during the pancreatic phase of the dynamic study shows a hypodense lesion in the head of the pancreas (arrow), representing a small adenocarcinoma at surgico-pathological examination. All images courtesy of Dr. Riccardo Manfredi."One of the major challenges for diagnostic imaging in oncology is represented by lymph node characterization, which is limited by the fact that the criteria for characterization is size; the threshold of 1 cm determines whether we discern a metastatic lymph node from a benign inflammatory lymph node," said Dr. Riccardo Manfredi, associate professor of radiology at the University Hospital of Verona, Italy, and moderator at today's session. "This means that normal size lymph nodes, with small metastatic implants of under 5 mm, are missed. Conversely inflammatory lymph nodes may enlarge and erroneously be considered malignant."
Organ-specific contrast agents and diffusion-weighted imaging, currently being explored in research, may improve lymph node characterization, but exactly how they will help is still under evaluation, he added.
 Serous cystadenoma: Axial half-Fourier T2-weighted image (TR/TE ∞/120 msec) shows a multicystic, microcystic neoplasm of the head of the pancreas with a central scar.
Serous cystadenoma: Axial half-Fourier T2-weighted image (TR/TE ∞/120 msec) shows a multicystic, microcystic neoplasm of the head of the pancreas with a central scar."With these limitations in mind, it is important for the radiologist to indicate to the surgeon the presence, site, and size of locoregional lymph nodes so that a histologic examination can be performed, which represents the gold standard in this setting," said Dr. Claudio Bassi, chair of the surgical department, University Hospital of Verona, Italy, who will speak today about the criteria for resectable and nonresectable pancreatic adenocarcinoma, treatment planning of neuroendocrine tumors, and the surgical indications in cystic pancreatic tumors.
Of vital importance in pancreatic management is whether or not the tumor is locally advanced. Vessel wall infiltration will often contraindicate surgery, but it remains difficult to distinguish infiltration from neoplastic tissue or benign inflammatory or desmoplastic reaction, when there is contact between the tumor and the vessel. Delegates can learn about the pathological criteria for vessel wall infiltration and the pattern of perivessel infiltration from Dr. Giuseppe Zamboni, chair of the pathology department at Negrar Hospital, Verona, Italy. His presentation about the added value of the pathologist will cover the features of different pancreatic neoplasms, as well as the histopathological findings that enable tumor characterization and those that show prognostic relevance.
The oncological issue of infiltration affects pancreatic tumors in particular. When assessing preoperative tumor respectability, the most frequent and important question for the surgeon is the relationship between the tumor and the adjacent vessel in order to understand whether the tumor can be separated from it, Manfredi explained. When fat can be detected between the vessel and the tumor, the tumor can be resected, but when the vessel is totally encased by the tumor, it can't. These two extreme examples represent the relatively easy cases, but in the majority of cases in which there is contact between the vessel and the tumor, it is difficult to preoperatively predict whether the surgeon will be able to pass his or her finger between the two, enabling resection, he noted.
"From the pathological point of view, the nature of the tissue responsible for the contact is the main determinant, with direct tumor contact most likely rendering it nonresectable. If contact is made through inflammatory/desmoplastic reaction, it is most likely to be resectable," said Manfredi, emphasizing that Zamboni's input is needed for more difficult cases.
Cases in Verona are discussed collegially every week. A resident presents the case's clinical history, laboratory findings, and other relevant data. The radiologists describe imaging findings, while the surgeons or gastroenterologists suggest treatment options.
"Each patient is discussed with different aims: Sometimes the diagnosis is not known and the challenge is in narrowing down the differential diagnosis; for others, the treatment options are debated, or the case is reviewed after the pathological diagnosis is obtained. In some cases, particular complications are discussed," Manfredi remarked.
This approach will be demonstrated during the panel discussion at today's session, in which the experts will guide the general radiologists present in the auditorium in the interpretation of example cases and show the strategies they employ to arrive at the correct diagnosis. Manfredi aims to outline the imaging findings in different pancreatic neoplasms, radiology's role of in surgical planning, and the strengths and weaknesses of imaging in patient management.
A case in point that determines management is whether pancreatic lesions are solid or cystic. A solid lesion must be resected, if possible, according to Bassi, while some cystic lesions can be followed up, as will be covered more fully by Zamboni, who will illustrate the different pathological patterns of pancreatic neoplasms, cystic and solid, their immunohistochemistry, and the possible progression from benign to malignant pancreatic tumor.
Depending on the indication, different surgical procedures for determining whether the lesion is a neoplasm or not mean different questions exist for the pathologist and the radiologist. The pathologist should know the criteria helpful for the differential diagnosis with tumor-like conditions that do not require surgery but medical therapy instead, while radiologists should know the diagnostic imaging signs for differential diagnoses in patients with a mass in the pancreas, Manfredi commented.
Originally published in ECR Today March 1, 2012.
Copyright © 2012 European Society of Radiology